With delayed parenthood now the norm, a new wave of biotech innovators is targeting the root cause of rising infertility rates. Oxford-based startup Uploid tells Femtech World how addressing egg ageing could reduce the “age penalty” that currently defines fertility outcomes.
Infertility now affects an estimated one in six people worldwide, with the World Health Organization determining it to be a “major public health issue.”
Across the OECD, the average age of first-time mothers has risen consistently over the past decades, driven by economic pressures, career progression, delayed partnership, and the availability of contraception. But human biology has not kept pace with this societal shift.
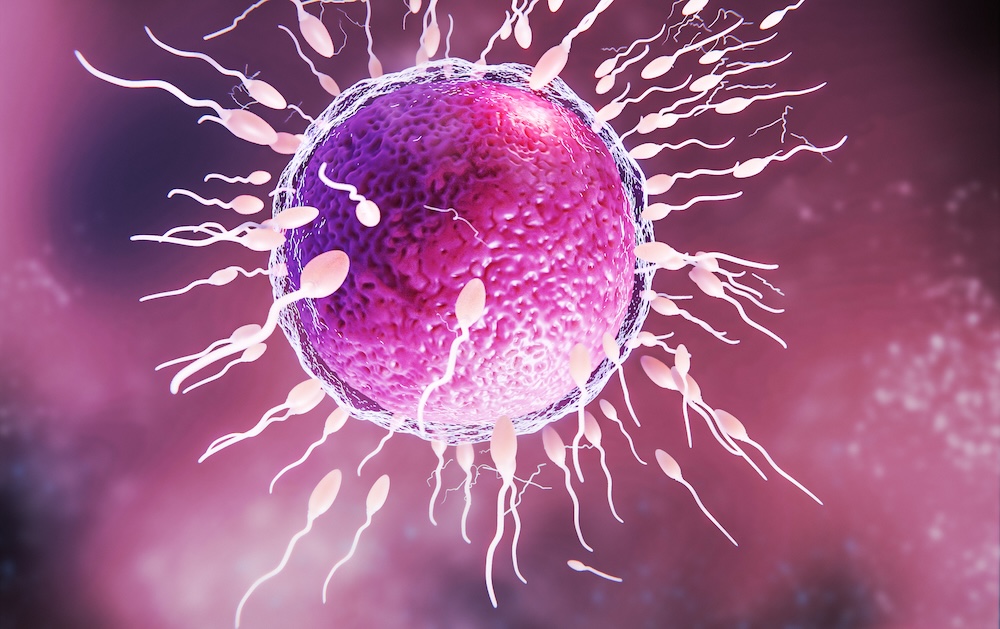
Egg quality declines sharply with age, beginning as early as the mid-thirties. It is this decline, not the body’s ability to carry a pregnancy, that remains the most significant factor behind falling conception rates.
IVF attempts to work around this challenge, yet even with technological advances, success rates remain modest. For women aged 18-34, birth rates per embryo transfer were around 35 per cent in 2022, dropping to five per cent by the age of 43-43.
“Fertility outcomes fall, not because the body is unable to sustain a pregnancy, but because egg quality declines with age,” Dr Alexandre Webster, co-founder and chief scientific officer at Oxford-based biotech firm, U-Ploid, tells Femtech World.
“Most existing fertility treatments are limited in how directly they can address this biological constraint. While IVF has advanced significantly in helping clinicians identify embryos with the best chance of success, there are currently very few options to intervene earlier and improve the quality of the eggs themselves.”
Current fertility treatments tend to focus on hormonal stimulation to produce more eggs, improving embryo selection, or improving implantation rates through uterine optimisation.
But none of these approaches address the root cause of age-related infertility, which is the egg’s declining ability to divide its chromosomes correctly.
This unmet need has set the stage for a new generation of reproductive biotech innovators, focusing on novel therapeutics, cellular engineering, AI-driven diagnostics, and biomarkers that could change how infertility is understood and treated.
A new frontier in fertility treatment
Among these innovators, U-Ploid is pioneering a new therapeutic category with Lyvanta™, a first-of-its-kind drug aimed at improving egg quality by addressing the biological mechanisms of maternal ageing.
Central to its approach is meiotic aneuploidy, which occurs when chromosomes fail to separate correctly as an egg matures. This increases dramatically with age, Webster explains, and is the leading cause of failed IVF cycles, miscarriage, and natural infertility. Studies have shown that over 50–80 per cent of embryos from women in their early 40s exhibit chromosomal abnormalities.
Lyvanta™ is designed to reduce the risk of these errors at the egg stage, before fertilisation occurs. It is injected into the egg before IVF, where it acts to stabilise chromosome segregation during meiosis.
“What makes this approach distinct is that, today, there are no approved or clinically available therapies that directly address meiotic aneuploidy or improve egg quality at its biological source,” Webster says.
“Lyvanta™ therefore represents a genuinely new therapeutic category. It does not act on embryos, does not alter DNA, and does not involve genetic modification. Instead, it supports a natural biological process that becomes increasingly error-prone with age.”
Evidence-gathering and regulatory engagement
The programme is grounded in over a decade of global academic research in chromosome biology and maternal ageing, and Uploid has carried out mechanistic studies, preclinical validation in aged animal models, and tightly regulated human egg studies in collaboration with IVF clinics.
However, the drug is still in the early stages of development, and the company is taking a cautious, evidence-driven approach.
Over the next one to two years, the research team will focus on building the scientific evidence needed to demonstrate clinical safety and efficacy. Meanwhile, regulatory engagement is ongoing, and timelines will depend on the outcomes of these studies.
“As with any new therapeutic, progress toward the clinic requires careful, stepwise evidence generation and regulatory review,” Webster says.
“Our focus at this stage is on ensuring that any future progress happens within established scientific, ethical, and regulatory frameworks. We engage with regulators, clinicians, and patient stakeholders to understand expectations around safety, evidence, transparency, and consent, and to ensure that the questions being asked of a new reproductive therapeutic are addressed rigorously and appropriately.”
He adds: “Lyvanta™ will only move forward if it meets the required standards set by regulators and ethics bodies, and only following thorough evaluation.”
If successful, the impact could be considerable. Improved egg quality may mean fewer IVF cycles, more viable embryos, and overall better outcomes for patients.
“If a therapy like Lyvanta™ can safely improve egg quality, it could lead to more viable embryos per IVF cycle, fewer cycles needed to achieve pregnancy, and better outcomes for people whose chances of success currently decline sharply with age,” Webster says.
“While much work remains, this is the long-term impact we are working toward.”
Global access and affordability
Globally, infertility affects people at similar rates regardless of income, but access to advanced treatments is often dependent on financial barriers.
IVF remains expensive worldwide. In the UK and US, a complete IVF cycle typically costs several thousand to tens of thousands of pounds, often requiring multiple attempts.
“One of the reasons fertility treatment is so costly and emotionally taxing is that patients often require multiple IVF cycles to achieve a successful outcome,” says Webster.
“Indeed, some 70 per cent of couples that start an IVF journey will end it with no baby, having run out of money and patience before a successful outcome.
By making each IVF cycle more efficient, it could reduce some of these costs and make treatment more accessible to more people.
“By improving egg quality upstream, Lyvanta™ has the potential to increase efficiency per cycle, which could reduce the overall burden, financial, physical, and emotional, on patients and healthcare systems,” Webster says.
The therapy is also being designed to integrate into existing IVF workflows, without requiring new infrastructure or highly specialised equipment.
He adds: “By focusing on improving biological efficiency rather than adding complexity, we believe this approach has the potential to support broader access over time, including in low- and middle-income countries where need is high but resources are limited.”
The new wave of fertility innovation
U-Ploid is part of a new wave of fertility biotech innovators. Companies such as Oxolife, developing a first-in-class oral drug to improve implantation; Gameto, engineering ovarian support cells to optimise IVF and egg freezing; and Genie Fertility, uncovering molecular biomarkers to personalise reproductive care, are all reshaping the field.
While progress in the fertility space has been incremental for decades, breakthroughs in chromosome biology, cell engineering, and molecular therapeutics are changing what might be possible.
This new generation of therapeutic innovation could improve outcomes and expand options for millions navigating delayed parenthood, and allow fertility science to catch up with the realities of modern life.
“Our aim is to reduce the biological ‘age penalty’ that currently defines fertility outcomes, so that success is less tightly coupled to chronological age,” Webster adds.
“If successful, this could allow more people to build families on timelines that reflect modern social and economic realities.”
link

