Oct. 04, 2024

The goal of peripartum pelvic physical therapy and occupational therapy is to reduce the long-term sequelae associated with postpartum pelvic floor dysfunction and to optimize and expedite return to function. To do this effectively, Nikki J. Ron, P.T., D.P.T., WCS-ABPTS, a physical therapist at Mayo Clinic in Rochester, Minnesota, urges clinicians to be mindful of the significant body changes that patients have experienced during pregnancy and childbirth.
“From a musculoskeletal perspective, women who have gone through pregnancy and childbirth are athletes,” says Dr. Ron. “Daily tasks for parents include lifting, squatting, carrying wiggly 20-pound toddlers, and they need care specific to the muscles that were torn, stretched and disrupted during pregnancy and delivery in order to perform those athletic endeavors appropriately.”
Using that knowledge, a multidisciplinary team headed by urogynecologic surgeon Annetta M. Madsen, M.D., has pushed for physical medicine and rehabilitation to be a vital part of the evolving peripartum pelvic health services, along with obstetrics, urogynecology and patient education. The hope is that by providing patients with early access to pelvic health physical and occupational therapy services through and immediately after pregnancy, they will normalize seeking and receiving these services throughout their patients’ life spans. “Early treatment for musculoskeletal conditions is always simpler and better, and we suspect that fewer visits will be needed overall if care can be initiated early,” explains Dr. Ron.
In this article, Dr. Ron shares details about the range of services the therapy team provides in the prenatal, acute postpartum and outpatient settings, and she describes some related research efforts that will help this field continue to evolve.
Prenatal pelvic healthcare
Prenatal therapy visits are prioritized for patients who are symptomatic. The most important type of referral is for patients suffering from pelvic girdle and low back pain. “We hope to get them in for treatment rapidly, as earlier care should allow moms to stay comfortable and active throughout pregnancy,” explains Dr. Ron. “Another important type of referral is for patients with urinary incontinence, as some of the best available evidence demonstrates that practicing Kegels correctly during pregnancy can help reduce the rates of incontinence postpartum.”
The team also provides birth prep consults, where they can answer any musculoskeletal questions, and questions about pushing and breathing strategies for labor and delivery positions, information that is especially useful for first-time moms and patients with preexisting orthopedic conditions. During a birth prep consult, team members also can address optimal bowel and bladder emptying strategies, as well as pelvic floor muscle contraction (Kegel) training to prevent or reduce the risk of urinary incontinence. They also may introduce perineal massage to help build patients’ pelvic floor muscle relaxation skills.
Acute postpartum pelvic healthcare
The team offers every mom a visit during the postpartum hospital stay, prioritizing patients who have undergone cesarean sections and patients with complex wounds and early signs of pelvic floor injury. Goals of acute care therapy are primarily to improve the patient’s function and mobility by reducing pain and improving muscular recruitment patterns immediately after birth. The hospital visit also includes a review of appropriate postures, with particular focus on incision protection. Therapists may monitor patient vital signs during functional tasks, encouraging safe and early mobility. Most importantly, the staff initiates the continuum of postpartum care by discussing outpatient pelvic therapy or follow-up with urogynecology.
Outpatient postpartum pelvic healthcare
The team offers all patients an outpatient pelvic health evaluation after childbirth. During a typical visit, which can be performed in person or via telehealth, the team assesses the patient’s posture, back and hip mobility, core and hip strength, pelvic floor function, and overall functional mobility. The team also screens for diastasis rectus abdominis and pelvic dysfunction.
Dr. Ron explains that the team encourages referrals of patients who are asymptomatic, so they can address how to optimize strength and posture to prepare for a return to heavy-lifting and high-impact activities. “We know that even patients who are asymptomatic have altered muscle recruitment patterns after labor and delivery, and often these are suboptimal. If we can help patients reeducate their muscles in a one-time consult visit immediately after birth, as their newborn grows and they return to high-level fitness, they should be more protected from injury.”
Referrals for postpartum physical therapy also are encouraged for any patients experiencing incontinence, pain (pelvic girdle, back, hip, coccyx, incision or dyspareunia), prolapse, constipation or diastasis rectus abdominis.
PFPT treatment options
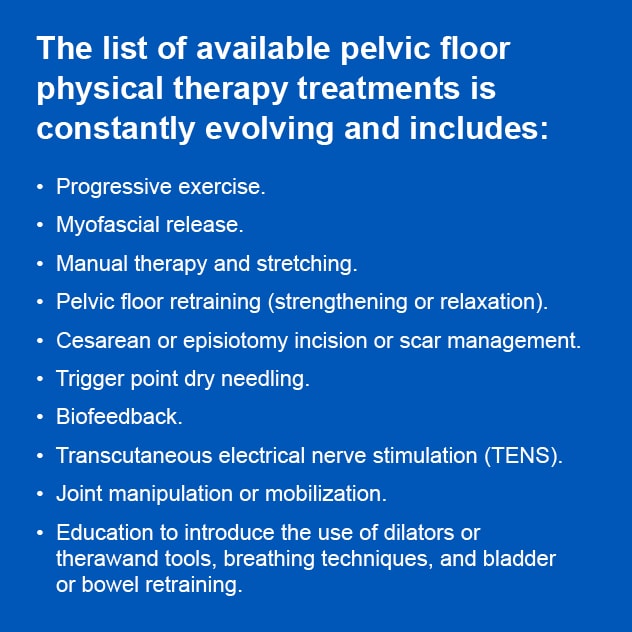
What happens during pelvic floor physical therapy (PFPT)? Dr. Ron notes that the team has a variety of treatment options and modalities at its disposal to help reach patient goals, including but not limited to the list shown at right. Many patients require only one visit for muscle reeducation. But for patients with underlying conditions or patients simply needing more support, 1 to 2 visits per week may be appropriate.
Research efforts
In a study published in the Journal of Women’s & Pelvic Health Physical Therapy in 2024, Dr. Ron and colleagues published the results of a study analyzing associations between running mechanics, functional lower extremity strength and stress urinary incontinence (SUI) in parous female runners. In that study, Dr. Ron and co-investigators concluded that parous female runners with more severe SUI and prolapse symptoms had altered running mechanics characterized by prolonged ground contact times and slower cadences. Dr. Ron and colleagues also have completed a preliminary study, currently awaiting publication, using transabdominal ultrasound in training of the pelvic floor muscles immediately after vaginal delivery.
For more information
Ron NJ, et al. Associations between running mechanics, functional lower extremity strength, and stress urinary incontinence in parous female runners. Journal of Women’s & Pelvic Health Physical Therapy. 2024;48:147.
Refer a patient to Mayo Clinic.
link




More Stories
One of the largest psychotherapy trials in the world has implications for transforming mental health care during pregnancy and after birth
Navigating Skin Disease Treatment During Pregnancy
CBT-I During Pregnancy Improves Sleep and Reduces Postpartum Depression