Survey study
Of the 305 healthcare providers (77 doctors and 228 nurses) who responded to the questionnaire, 286 completed the TSQ. Among the 286 respondents, the PTSS group comprised 178 respondents (62.2%) and the probable PTSD group 52 respondents (18.2%). Of those who responded that CPR was a traumatic event, 115 (40.2%) were in PTSS group and 32 (11.2%) in probable PTSD group. In the probable PTSD group, wherein the participants were positive for PTSD as per the diagnostic screening test, the odds ratio between developing PTSD due to CPR and events other than CPR was 3.02 (p-value < 0.05).
The trauma symptoms after administering CPR occurred significantly more frequently in nurses than in doctors, in both the PTSS (75.7%vs. 24.3%, p = 0.049) and probable PTSD groups (90.6% vs. 12.5%, p = 0.013). Regarding trauma symptoms occurrence, there was no difference according to the title held by the doctors; however, there was a statistical difference according to the nurses’ years of experience. Nurses with 2–5 years of experience were most likely to experience trauma symptoms after performing CPR in both the PTSS (35.6%, p < 0.05) and probable PTSD groups (48.3%, p < 0.05). The total number of CPRs performed and locations where they were performed were significantly different only in the PTSS group (p = 0.045 and 0.031, respectively). In the PTSS group, those who performed CPR more than ten times comprised the largest group (64.3%), whereas those who performed CPR only once, comprised the fewest group (7.0%). The most common location where CPR was performed was the general ward (36.5%), followed by the emergency room (13.0%; Table 1).
Most people with trauma symptoms responded that they endured them without taking any special action (44.5%), talked to acquaintances such as family, friends, and colleagues, (44.5%), or took a break from work (29.7%; Fig. 1). Even in the probable PTSD group, only one participant answered that they had consulted an expert.
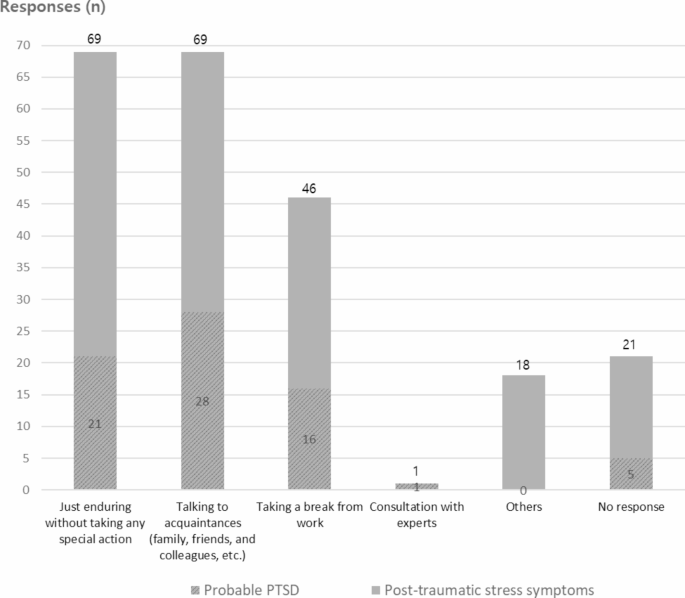
Measures reported by the participants to address trauma symptoms (multiple responses were possible).
Qualitative interview study
Eight healthcare providers (two doctors and six nurses), participating in this study, were interviewed regarding their experiences of administering CPR that caused them to develop trauma symptoms. Following the content analysis, four themes with twelve subthemes emerged (Table 2).
1) Healthcare providers unprepared for CPR.
The participants responded that they experienced trauma symptoms after they performed CPR in unexpected situations, such as when the patient’s condition before the cardiac arrest occurred was relatively stable or when the cardiac arrest was not immediately recognized and discovered at a later stage. In addition, most participants reported that they had not received proper CPR training, had little actual experience, and had not performed CPR for a long time.
1.1) Unexpected cardiac arrest
Participant 1: The patient was in an isolation room. The monitor was not working, so I went to check and found that the patient was in cardiac arrest. No one knew for how long he was in that state.
Participant 2: The patient came just to check if his coronary arteries were okay or not. So, I was under the impression that it would be over soon, but as soon as the intervention started, a sudden cardiac arrest occurred…I performed CPR without any preparation.
1.2) Absence of proper CPR training
Participant 1: There is no training in neonatal CPR at the hospital. I just learn from experience, study on my own, or listen to the preceptors. That is all.
1.3) Lack of CPR experience
Participant 2: I was doing CPR for the first time. So, I could not prepare the medicine properly because my hands were shaking.
Participant 7: Since this is only my second CPR, I do not know what to do….
2) Difficulties faced during CPR administration.
The participants responded that they experienced trauma symptoms when faced with several difficulties during CPR. They felt that the CPR process was very difficult when they could not perform their roles properly or lacked manpower. Furthermore, they stated that it was difficult to see patients who were vomiting blood or had broken ribs. They were also skeptical when they continued to perform meaningless CPR on a patient with less likelihood of resuscitation.
1.1) Not performing their role properly
Participant 1: The professor came and asked whether the blood test had been done; I had not done it. I only checked the patient’s pulse and saturation, and then I measured blood pressure, did a blood test, and gave bicarbonate….
Participant 6: Another nurse gave epinephrine, not intravenously but intra-arterially. The blood was flowing backward, but she was flushing by giving epinephrine.
1.2) Shortage of CPR providers
Participant 2: I think it was overwhelming because I had to make all the ECMO preparations, priming, intubation, and drugs by myself. I had too many things to do….
1.3) The patient’s morphology is unsightly
Participant 4: I still cannot forget the image of the patient’s ribs breaking and him vomiting blood during CPR. And the patient was also undressed.
Participant 6: A lot of blood came out while suctioning, but the smell was so disgusting. When I came home and washed my body, the smell of blood kept coming into my nose, blood was all over my body, and there was blood all over the sheets and floor… that later appeared in my dream.
1.4) Skepticism about continuing meaningless CPR
Participant 4: I thought it would be better not to do CPR for so long.
Participant 5: Most cardiac arrest people do not get resuscitated, or even if they do, their quality of life is very poor. So I had a lot of doubts about whether I should do CPR. I think that if I had a cardiac arrest, I would never want to receive CPR.
3) Negative emotions after performing CPR.
The participants suffered from negative emotions such as guilt toward the patient’s family for not being able to save the patient’s life, self-blame over whether the patients might have survived if they had done better or if someone else had performed CPR, and fear of experiencing a similar CPR situation again.
1.1) Guilt toward the patient’s family
Participant 2: First of all, I felt sorry for the family. They trusted us and entrusted the patient to us, but he passed away after not being properly treated. They kept crying… The professor was explaining, but they just cried… I was so sorry.
1.2) Blaming themselves
Participant 3: Although she was in distress, I thought she would be able to endure it because she was young. I think I was greatly mistaken…I think she might have survived if she had been treated by someone other than me.
Participant 8: In fact, there is such a thing as guilt that I wish I had done better when intubating him at that time and given him a little more oxygen.
1.3) Fear of re-experiencing
Participant 5: Every time I went to work, I felt very burdened that the patient would get worse. When CPR is required, even if a helper comes from other wards, I think there is anxiety that the patient is getting worse.
Participant 7: When patients of the same age or with similar diagnoses were hospitalized, it was a bit… I think there was something frightening about it for no reason…It was mentally difficult to cope with an emergency like this, and I thought a lot that my skills were not so good.
4) Overcoming stress and moving forward.
The participants responded that after overcoming trauma symptoms, they paid more attention to their patients and made more efforts to take better care of them than before experiencing trauma symptoms. And they reported debriefing after CPR was helpful in overcoming trauma symptoms.
1.1) Providing better care to patients
Participant 7: There are a lot of bedridden people. I did not pay much attention to their mental status before, but recently, I think I pay more attention to them. In some ways, it may have been an opportunity for me to do better nursing….
1.2) Debriefing on CPR helps to overcome stress
Participant 2: Talking about CPR, such as “This could have happened because of this,” or” I wish it had happened sooner,” etc. helps prepare for the next CPR.
link






More Stories
Recovery-oriented and trauma-informed care for people with mental disorders to promote human rights and quality of mental health care: a scoping review | BMC Psychiatry
Best Healthcare Destinations for AI-Powered Post-Trauma Recovery | Medical Tourism Magazine | Medical Travel
New Study Examines Patient Suicide and Its Toll on Providers