1 Introduction
Since the outbreak of the coronavirus disease 2019 (COVID-19) in 2019, more than 30 million confirmed cases have been recorded in South Korea (1). Although several studies investigated the psychological repercussions of Severe Acute Respiratory Syndrome in 2002 and the Middle East Respiratory Syndrome in 2013, during the 3 years of COVID-19, there has been a marked gap in empirical research needed to prevent psychological burnout and protect the mental health of healthcare professionals working at the frontlines of the pandemic. It is important to note that PTSD and PTG can be found simultaneously in individuals (2–4). This indicates that these concepts are not entirely opposing phenomena and suggests that both may occur together during the pandemic. We employ a positive psychological approach, focusing not simply on minimizing the suffering and side effects but going beyond to overcoming the crisis and utilizing it as an opportunity for personal growth and development. Posttraumatic growth (PTG) refers to positive qualitative changes attained after a crisis beyond merely recovering to the pre-crisis level (5). It is not only a product of overcoming trauma but also serves as a protective factor against burnout, thus enhancing resilience (6).
In a study on tertiary hospital nurses who provided direct patient care during the pandemic, Lee et al. (7) reported that 63.9% of nurses had experienced PTSD, while 49.7% had clinical depression. A meta-analysis on the prevalence of PTSD during the COVID-19 pandemic reported that, in particular, nurses who provided direct patient care were experiencing high levels of stress and a high prevalence of PTSD (8). In addition, Martin et al. (9) reported that a high workload and unprecedented levels of burnout (BO) during the pandemic caused substantial levels of stress among the US nursing population, particularly among the younger and less experienced nurses, leading to an overall 3.3% decline in the I.S. nursing workforce over a 2-year period. The issues related to this work overload appear to be consistent not only among nurses directly handling infected patients but also among administrative staff (10). These results suggest that nurses in clinical practice would be affected by serious psychological BO and suffering. Healthcare professionals working at the frontlines of the pandemic faced higher levels of physical and emotional BO owing to more frequent exposures to pain from the loss of patients and colleagues and frequent infection risks (11), with the highest rate of BO reported among nurses (12).
A study on nurses’ PTG during the COVID-19 pandemic showed that nurses at the frontlines experienced moderate-to-severe psychological stress responses and that COVID-19-related stress leads to positive changes through deliberate rumination (13). In addition, studies have reported that PTG is negatively associated with psychological distress in frontline healthcare professionals (14). According to a study on the impact of PTG on psychological distress after COVID-19, the level of depression and anxiety declines with increasing PTG (15), and PTG is negatively associated with psychological distress in frontline healthcare professionals battling COVID-19 (13). Moreover, Hamama-Raz et al. (16) reported that PTG is negatively proportional to BO caused by job-related stress in nurses. PTG is a term that not only signifies the enhancement of individual psychological resources or abilities but also denotes the process of coping strategies for severe stress (17). PTG can serve as a coping strategy to shield individuals from the impact of a pandemic, allowing them to emerge from distress intact. We infer that PTG has a protective potential against deteriorations of psychological health and BO in healthcare professionals facing extreme psychological distress from COVID-19.
Cognitive emotion regulation (CER) refers to cognitive coping strategies, which enable an individual to control and not be overwhelmed by their emotions due to threatening or stressful events (18). Garnefski and colleagues delineated nine specific cognitive strategies, namely acceptance, positive reappraisal, positive refocusing, refocusing on planning, putting into perspective, self-blame, blaming others, rumination, and catastrophizing. Subsequent empirical research, including a comprehensive meta-analysis by Aldao et al. (19), has demonstrated that maladaptive CER strategies such as self-blame, blaming others, rumination, and catastrophizing are more strongly associated with psychopathology than their adaptive counterparts and that mood-related disorders such as depression and anxiety disorders are more strongly connected to CER than other (20). Conversely, adaptive CER strategies, especially positive reappraisal, positive refocusing, and refocusing on planning, have shown positive correlations with PTG in studies by Im and Kwon (21) and Lee and Yang (22). Reflective rumination, examined by Cui et al. (13) and Romeo et al. (23), positively influences PTG in nurses. Research involving Korean nurses has consistently validated that deliberate rumination positively influences PTG (24, 25). According to the posttraumatic growth model of Tedeschi and Calhoun (26), individuals typically undergo intrusive rumination immediately after a traumatic event but ultimately achieve PTG through a process involving deliberate rumination, emotional recognition and expression, and social support. This pathway has been validated by Morris and Shakespeare-Finch (27) and Taku et al. (28). Emotional expression following trauma, as indicated by Manne et al. (29) and Song and Lee (30), facilitates PTG.
Moreover, social support is sometimes described as the major environmental resource influencing PTG (31). Ogińska-Bulik et al. (32) reported a positive correlation between PTG and social support in healthcare professionals, including nurses, and Aliche et al. (33) reported in a study on young adult terrorism survivors that social support directly increases PTG. A meta-analysis (34) of 217 studies shows a consistent positive relationship between social support and PTG, significant in both longitudinal and cross-sectional studies. In addition, Žukauskienė et al. (35) reported that social support predicts a higher level of PTG in victims of domestic violence by a spouse. These findings suggest that social support has an impact on PTG.
Factors known to affect PTG, namely CER strategies, deliberate rumination, and emotional expression, not only facilitate positive changes following a traumatic experience but also alleviate negative symptoms such as anxiety, depression, and BO. BO is a response arising from stressful events characterized by emotional exhaustion, reduced personal accomplishment, and a negative or cynical attitude toward others (36). Previous research indicates that adaptive CER negatively impacts BO (37) and generalized anxiety (38). Therefore, adaptive CER appears to potentially reduce the negative effects resulting from stress events, such as BO. Reflective rumination can reduce symptoms of depression, anxiety (39), and the risk of stress-related symptoms and BO (40) by promoting the processing of information and meaning related to traumatic events. This aligns with previous findings suggesting that deliberate thinking about traumatic events can mitigate psychological distress by modifying pathological thought patterns (41, 42). Hence, we can infer that the positive benefits of deliberate rumination could apply to healthcare professionals who experienced the COVID-19 pandemic distress as well.
Expressing one’s emotions toward a traumatic experience reduces anger, tension, and depression in trauma survivors (43), while suppressing emotions increases anxiety, depression, and PTSD symptoms (PSs) (44, 45). These results have also been documented in a study on nurses’ BO. In a study of clinical nurses in Korea, Park (46) reported a negative correlation between emotional expression and BO. In other words, the odds for BO were lower among nurses who express their emotions more often.
Based on the results of the literature review, we hypothesized that PTG facilitators will reduce BO and PS in nurses through the mediation of PTG. We aim to develop and validate a path model based on this hypothesis. PTG serves as a buffer against BO and PS, and causal variables that promote PTG, such as deliberate rumination, emotional expressivity, and adaptive CER, are included in the model. In other words, PTG acts as a mediator in the model. Additionally, we have considered covariates that influence psychological variables. For example, religion has been associated with high PTG in the Korean sample (47). While specific hypotheses regarding the effect of other covariates have not been established, considering the characteristics of participants and the specificity of the situations they are in would help in understanding the findings.
2 Materials and methods
2.1 Participants
An online survey using Google Forms was conducted from September to December 2022 with nurses of secondary hospitals and local hospitals in the provinces of Gyeonggi, Gangwon, and Chungcheong in South Korea. All participants were explained the study’s purpose, after which they signed an informed consent form. A total of 251 nurses were enrolled. Of these nurses, data from four participants were excluded because of having a value of p < 0.001 on the Mahalanobis distance (D2) test (48) or choosing only one response option on four or more instruments; data from 247 participants were therefore included in the final analysis.
The participants’ demographic characteristics are summarized in Table 1. Of all participants, 233 were female (94.33%) and 14 were male (5.67%). The mean age was 32.67 years (SD = 8.35, excluding one participant owing to no response). Other demographic characteristics assessed were marital status, religion, education, clinical career, type of work facility, and job position.
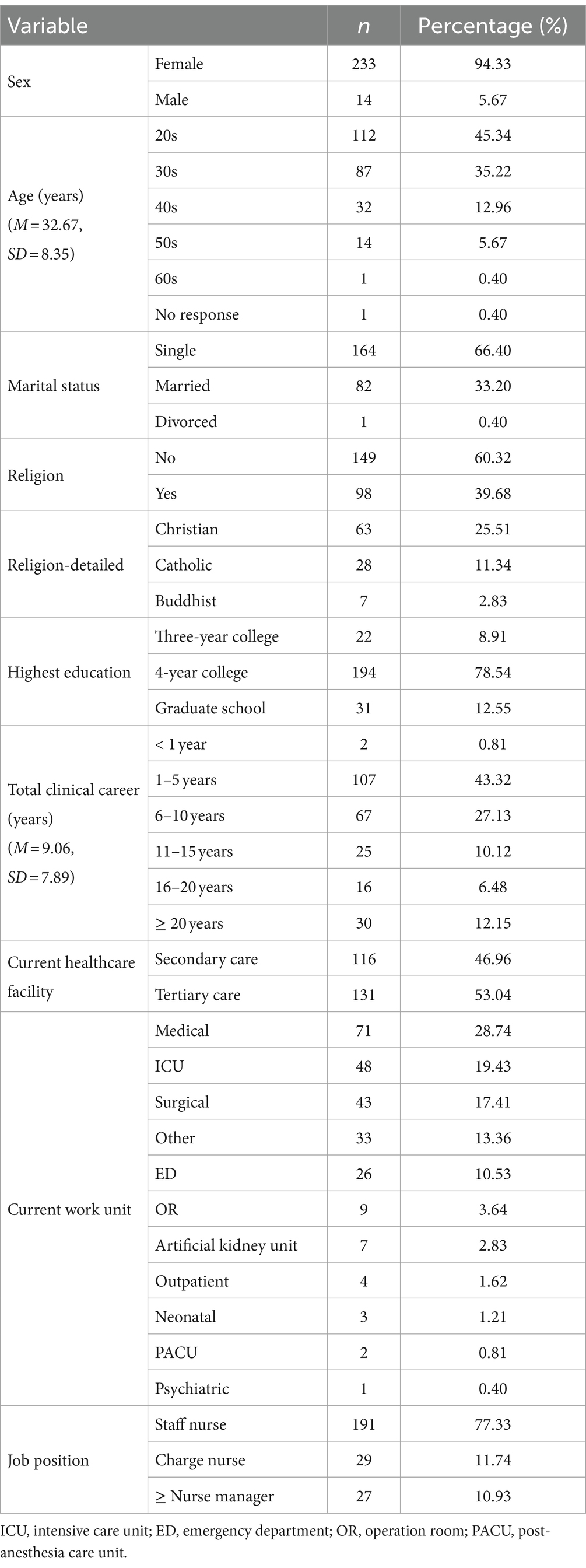
Table 1. Participants’ demographic characteristics (N = 247).
2.2 Instruments
2.2.1 Posttraumatic growth inventory
The Posttraumatic Growth Inventory (PTGI) was developed by Tedeschi et al. (49) to measure PTG—referring to growth attained following a painful experience beyond the pre-trauma levels. The original 25-item scale covers five domains. In our study, the PTGI-X, a Korean-translated and adapted version by Im (47), was used. The PTGI-X contains 18 items that assess three factors (changes of self-perception and personal strength, spiritual-existential change, and interpersonal relationship). The participants rate each item using a 6-point scale from 0 (never experienced) to 5 (experienced frequently). Aggregated scores range from 0 to 90, in which higher scores indicate more substantial growth. The internal consistency (Cronbach’s α) was 0.95 for the entire inventory and 0.82–0.94 for each factor in our study.
2.2.2 Burnout assessment tool
The Burnout Assessment Tool (BAT) is a self-report questionnaire developed by Schaufeli et al. (50) to measure BO and adapted and validated in Korean by Cho (51). The 22-item Korean version has one less item from the original tool, and each item is rated on a 5-point Likert scale (0 “never” to 4 “always”). Aggregated scores range from 0 to 88, in which higher scores indicate increased severity of burnout. Four factors are used: exhaustion, mental distance, impaired emotional control, and impaired cognitive control. The internal consistency (Cronbach’s α) was 0.93 for the entire inventory and 0.77–0.87 for each factor in our study.
2.2.3 PTSD checklist for DSM-5
The PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (PCL-5) is developed by Blevins et al. (52) to measure levels of PTSD symptoms occurring after a trauma event. We used the Korean version validated by Lee et al. (53). This 20-item scale is rated on a 5-point Likert scale. Aggregated scores range from 0 to 80, in which higher scores indicate more severe symptoms. The cutoff score for the Korean version of the PCL-5 is 26, and participants who scored above this point were classified as the PTSD group (54). This cutoff score is relatively lower than those observed in clinical populations in other studies, which suggest cutoffs of 41 (55) and 37 (56). The PCL was originally developed based on the diagnostic criteria of DSM-5, considering the four factors: intrusion, avoidance, negative alterations in cognition and mood, and hyperarousal. Recent empirical advancements, however, advocate for a seven-factor model of PTSD—re-experiencing, avoidance, negative affect, anhedonia, externalizing behaviors, anxious arousal, and dysphoric arousal—as providing a superior fit. This model, supported by both theoretical and empirical evidence, represents a significant evolution in having the best fit (54, 57, 58). The internal consistency (Cronbach’s α) was 0.95 for the entire inventory in our study.
2.2.4 Event-related rumination inventory
The Event-Related Rumination Inventory (ERRI) is a self-report scale developed by Cann et al. (59) to measure intrusive and deliberate rumination, which refers to repeated re-living of a shocking or painful event. There are 10 items for each factor, and each item is rated on a 4-point Likert scale. In the present study, we only used 10 items for deliberate rumination used in the Korean-validated version by Ahn et al. (60). Aggregated scores range from 0 to 30, in which higher scores indicate more deliberate rumination. The internal consistency (Cronbach’s α) was 0.94 for the deliberate rumination subscale.
2.2.5 Emotional expressivity scale
The Emotional Expressivity Scale was developed by Kring et al. (61) to measure emotional expression, which refers to the degree to which one expresses positive and negative emotions. In the present study, we used the scale translated by Han (62) after modifying it for the COVID-19 situation. This single-factor scale contains eight items, and each item is rated on a 5-point Likert scale. Aggregated scores range from 0 to 32, in which higher scores indicate more emotional expression. The internal consistency (Cronbach’s α) was 0.64 in this study.
2.2.6 Cognitive emotion regulation questionnaire
The Cognitive Emotion Regulation Questionnaire (CERQ) was developed by Garnefski et al. (18) to measure CER strategies for the regulation of emotions pertaining to an event. We used the Korean version validated by Ahn et al. (20). The tool contains 35 items, and each item is rated on a 6-point Likert scale. The scale includes two subscales: adaptive regulation (acceptance, putting into perspective, positive refocusing, refocus on planning, and positive reappraisal) and maladaptive regulation (self-blame, catastrophizing, other-blame, rumination, intrusive, and negative). Aggregated scores range from 0 to 70 for adaptive factors and from 0 to 55 for maladaptive factors. The internal consistency (Cronbach’s α) for the entire inventory was 0.95, and it ranged from 0.76 to 0.90 for sub-factors.
2.2.7 Multidimensional scale of perceived social support
The Multidimensional Scale of Perceived Social Support was developed by Zimet et al. (63) to measure positive resources that can be obtained from social relationships. This tool measures social support received from family, friends, or significant others, and we used the Korean version developed by Yune and Oh (64). This 12-item tool is rated on a 7-point Likert scale. Aggregated scores range from 0 to 72, in which higher scores indicate more considerable social support. The internal consistency (Cronbach’s α) was 0.95 for the entire inventory and 0.94–0.96 for each factor in our study.
2.3 Analysis
First, descriptive statistics were reported, and skewness and kurtosis of the variables were examined to assess the multivariate normality assumption.
Second, an analysis of variance (ANOVA) and t-test were conducted to explore covariates potentially affecting variables in the mediation model. These included demographics and COVID-19-related job characteristics. Post-hoc analysis for the ANOVA was conducted using Scheffe’s method.
Third, we conducted model comparisons to select the causal variables to be included in the mediation model. This step was taken to determine if the variables (deliberate rumination, emotional expression, adaptive CER, maladaptive CER, and social support) theoretically believed to predict PTG, BO, and PS based on existing literature statistically significantly predict PTG, BO, and PS and to ensure parsimony of the mediation model. Model comparison was carried out using the Type III Sum of Squares (SS) method, which involved comparing the full model with restricted models where each independent variable was omitted one by one to identify variables causing significant residual changes in the model. This method is useful for exploring significant variables regardless of the order of entry of independent variables and simplifying the model. To diagnose multicollinearity in each model, the variance inflation factor (VIF) was calculated. In the PTG regression model, adjusted generalized VIF [GVIF1/(2*df); (65)] was used due to the inclusion of a categorical independent variable of three levels (highest education). If the VIF exceeds 10 or the GVIF1/(2*df) exceeds 2, it is interpreted as an indication of multicollinearity (65, 66).
Finally, we validated the mediation model using the covariates and causal variables selected in the first and second steps. Since covariates were all categorical variables, they were dummy-coded, and they were set to estimate the effects on causal, mediating, and outcome variables. We used the robust maximum likelihood method, and missing data were processed with full information maximum likelihood (FIML). One item containing 38 missing values was from the Event-Related Rumination Inventory.
3 Results
3.1 Descriptive statistics and correlation analysis
Table 2 shows the descriptive statistics of major variables and the correlations among the variables. The absolute values of skewness for all variables were less than 2, and the absolute values of kurtosis were less than 7, meeting the criteria for multivariate normality suggested by Curran et al. (67). According to the cutoff score of PCL-5 (54), 47.81% of the participants in this study were classified as the PTSD group. PTG was not significantly correlated with BO (r = −0.10, p = 0.100) and PS (r = 0.02, p = 0.774) but was significantly positively correlated with deliberate rumination (r = 0.57, p < 0.001), emotional expression (r = 0.32, p < 0.001), adaptive CER (r = 0.54, p < 0.001), maladaptive CER (r = 0.28, p < 0.001), and social support (r = 0.23, p < 0.001). There was a strong correlation between BO and PS (r = 0.69, p < 0.001), and both were significantly positively correlated with deliberate rumination (BO: r = 0.21, p < 0.001; PS: r = 0.39, p = 0.002) and maladaptive CER (BO: r = 0.43, p < 0.001; PS: r = 0.56, p < 0.001) and significantly negatively correlated with social support (BO: r = −0.19, p = 0.003; PS: r = −0.25, p < 0.001).
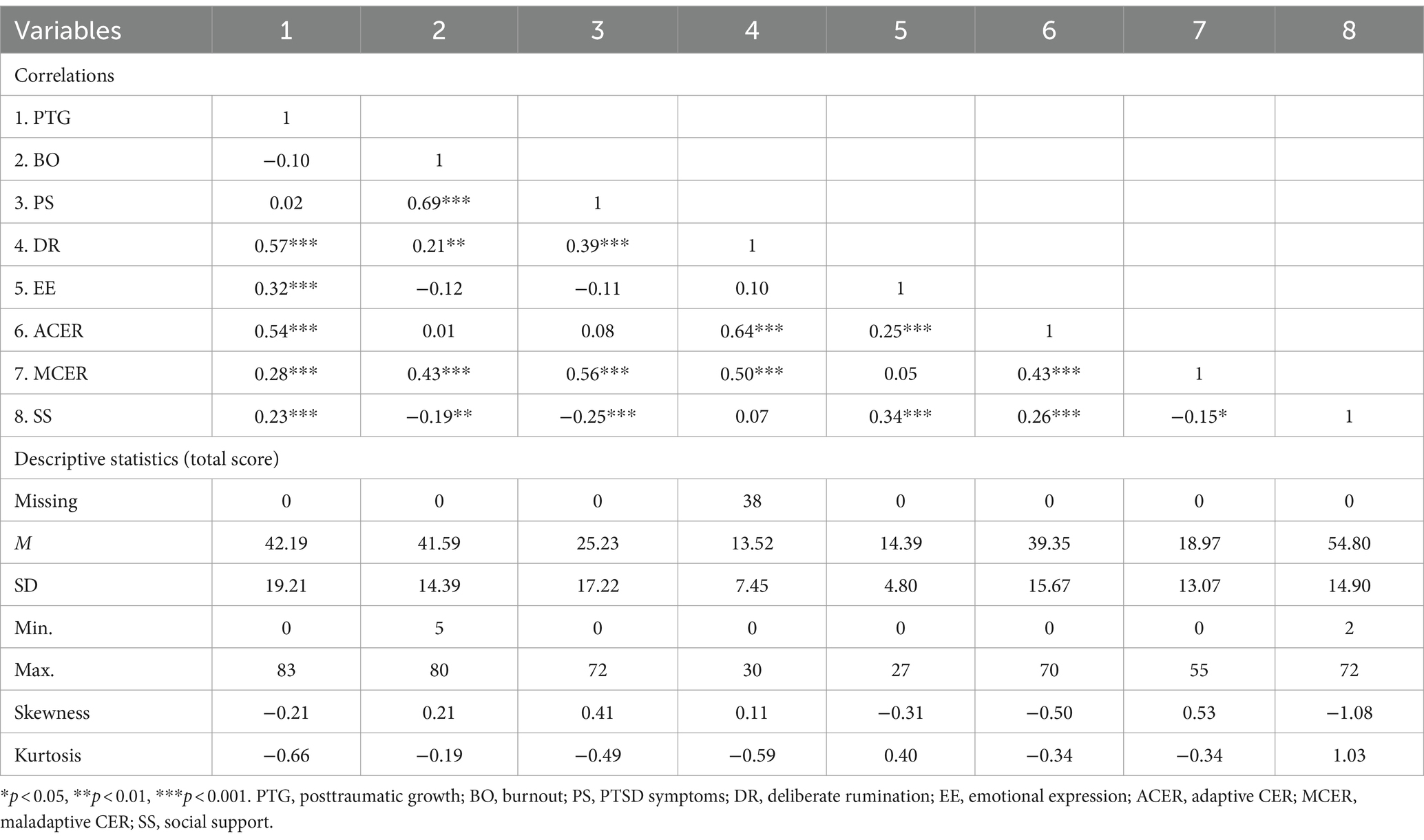
Table 2. Descriptive statistics and correlations.
3.2 Comparison of major variables according to demographic characteristics
According to demographic characteristics, the differences in the variables were analyzed using a t-test or ANOVA (Table 3). The results indicated that age, education level, religion, type of healthcare facility, current job position, prior work experience in a screening center, prior work experience in a residential treatment center, shift work during the COVID-19 pandemic, and prior completion of COVID-19-related infection control education had a significant effect on one or more study variables. More specifically, education level influenced PTG, F(2, 244) = 3.053, p = 0.049, η2 = 0.024, and religion influenced PTG, t(245) = −3.912, p < 0.001, d = 0.510, 95% C.I. [0.250, 0.768], BO, t(245) = 2.286, p = 0.023, d = 0.298, 95% C.I. [0.041, 0.554], and deliberate rumination, t(207) = −2.360, p = 0.019, d = 0.338, 95% C.I. [0.055, 0.621]; Type of healthcare facility influenced PTG, t(245) = 2.248, p = 0.025, d = 0.287, 95% C.I. [0.035, 0.538], and current job position influenced PTG, t(245) = −2.885, p = 0.004, d = 0.438, 95% C.I. [0.138, 0.738], BO, t(245) = 2.674, p = 0.008, d = 0.406, 95% C.I. [0.106, 0.706], PS, t(110.64) = 2.373, p = 0.019, d = 0.338, 95% C.I. [0.019, 0.618], and maladaptive CER, t(130.50) = 3.199, p = 0.002, d = 0.435, 95% C.I. [0.097, 0.697]. An imbalance in sample size across groups was found for certain variables, such as gender, making it difficult to test the effects of these variables.
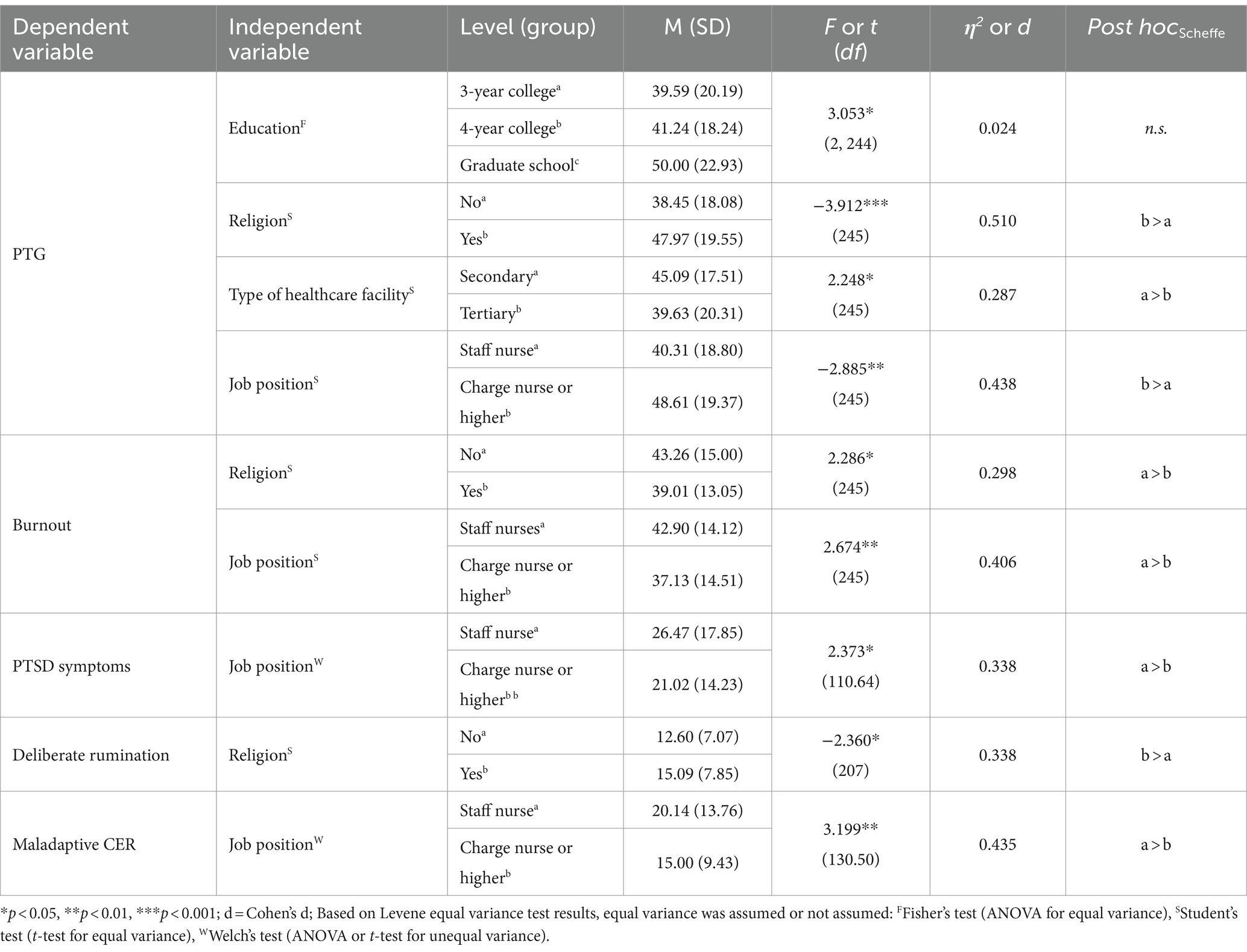
Table 3. Comparison of major measurement variables according to demographic characteristics (one-way ANOVA).
3.3 Predictors of PTG, BO, and PS
Table 4 shows the results of regression analysis to investigate the significant predictors of PTG, BO, and PS. PTG was statistically significantly influenced by religion, F(1, 198) = 6.153, p = 0.014, current job position, F(1, 198) = 5.880, p = 0.016, deliberate rumination, F(1, 198) = 26.772, p < 0.001, emotional expression, F(1, 198) = 15.673, p < 0.001, and adaptive CER, F(1, 198) = 6.620, p = 0.011. In the regression model for PTG, the GVIF1/(2* df) values ranged from 1.06 for the type of work facility to 1.41 for adaptive CER, indicating no multicollinearity issues. BO was statistically significantly influenced by PTG, F(1, 200) = 4.978, p = 0.027, deliberate rumination, F(1, 200) = 8.638, p = 0.004, adaptive CER, F(1, 200) = 7.297, p = 0.007, and maladaptive CER, F(1, 200) = 44.942, p < 0.001. PS was statistically significantly influenced by PTG, F(1, 201) = 3.966, p = 0.048, deliberate rumination, F(1, 201) = 25.691, p < 0.001, adaptive CER, F(1, 201) = 14.826, p < 0.001, and maladaptive CER, F(1, 201) = 67.298, p < 0.001. In the models for BO (VIF ranged from 1.10 for religion to 2.22 for deliberate rumination) and PS (VIF ranged from 1.12 for job position to 2.21 for deliberate rumination), there were no issues of multicollinearity.
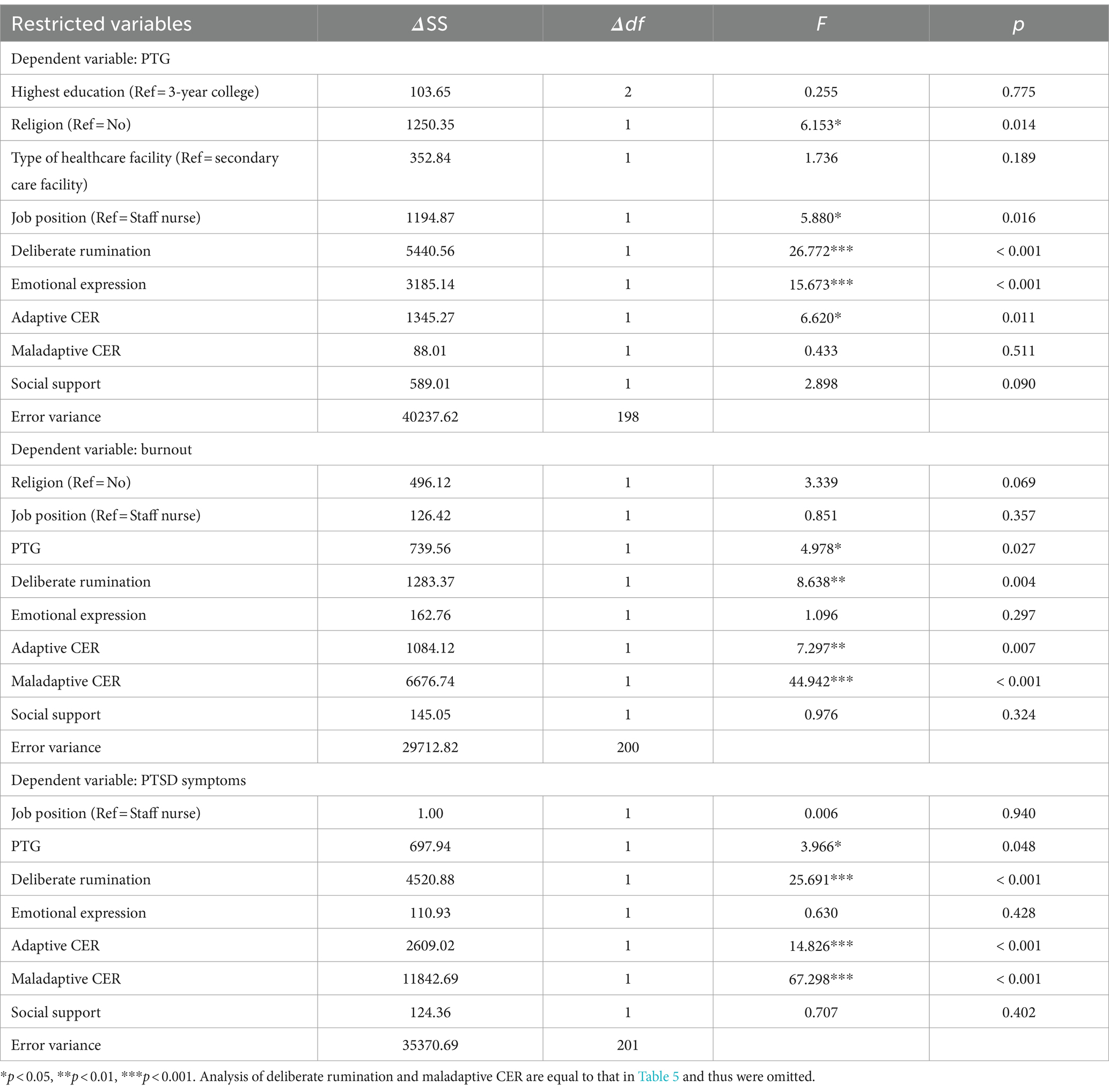
Table 4. Model comparison for PTG, burnout, and PTSD symptoms (type III method).
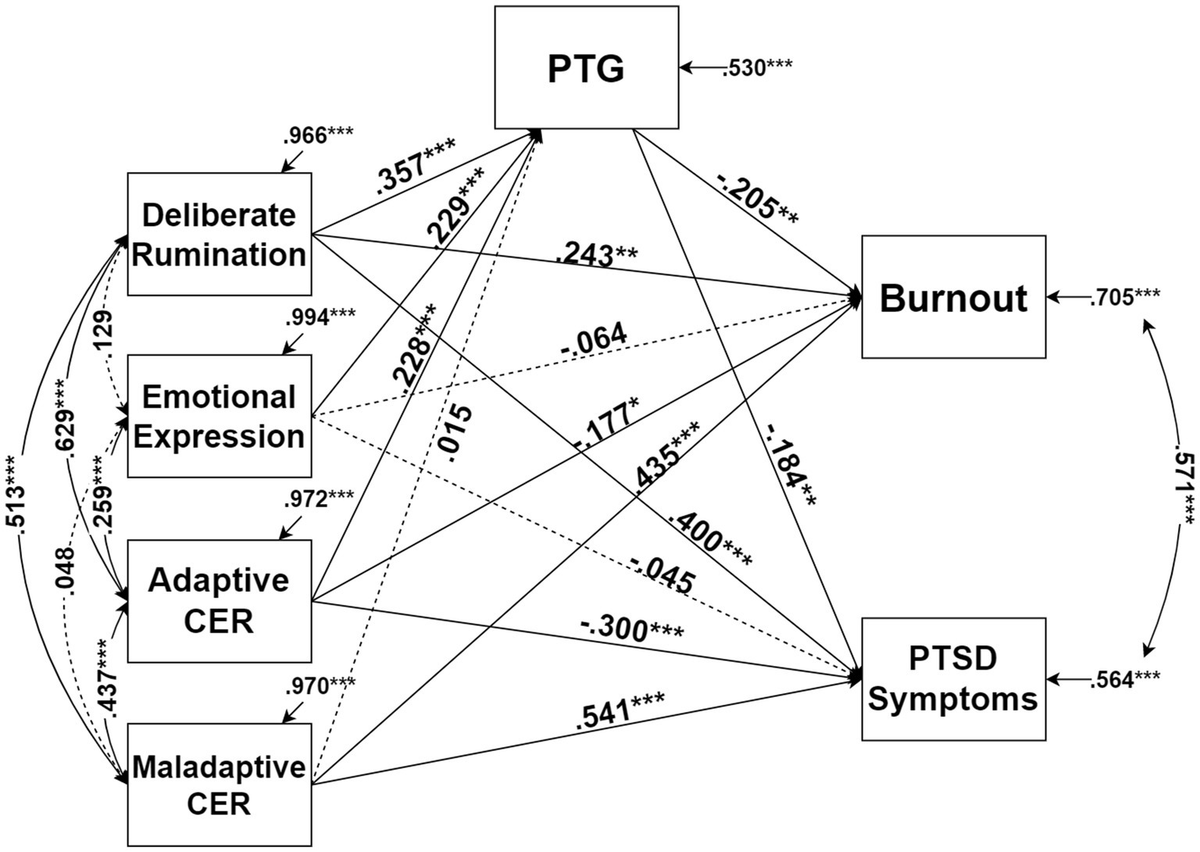
3.4 Validation of mediation model
Finally, we conducted a path model analysis to determine whether the predictors affect BO and PS through PTG with the inclusion of demographic variables in the model. The results of the mediation model analysis are shown in Figure 1 and Tables 5, 6. Bootstrapping (Table 6) was performed to statistically analyze the mediating effects. Deliberate rumination, emotional expression, and adaptive CER significantly predicted BO and PS with the inclusion of demographic variables in the model. The total effect of all causal variables on BO was significant (p < 0.05), and the total effect of all causal variables excluding emotional expression on PS was significant (p < 0.001). In summary, the effect of deliberate rumination and adaptive CER on BO and PS was partially mediated by PTG, and the effect of emotional expression was completely mediated by PTG.
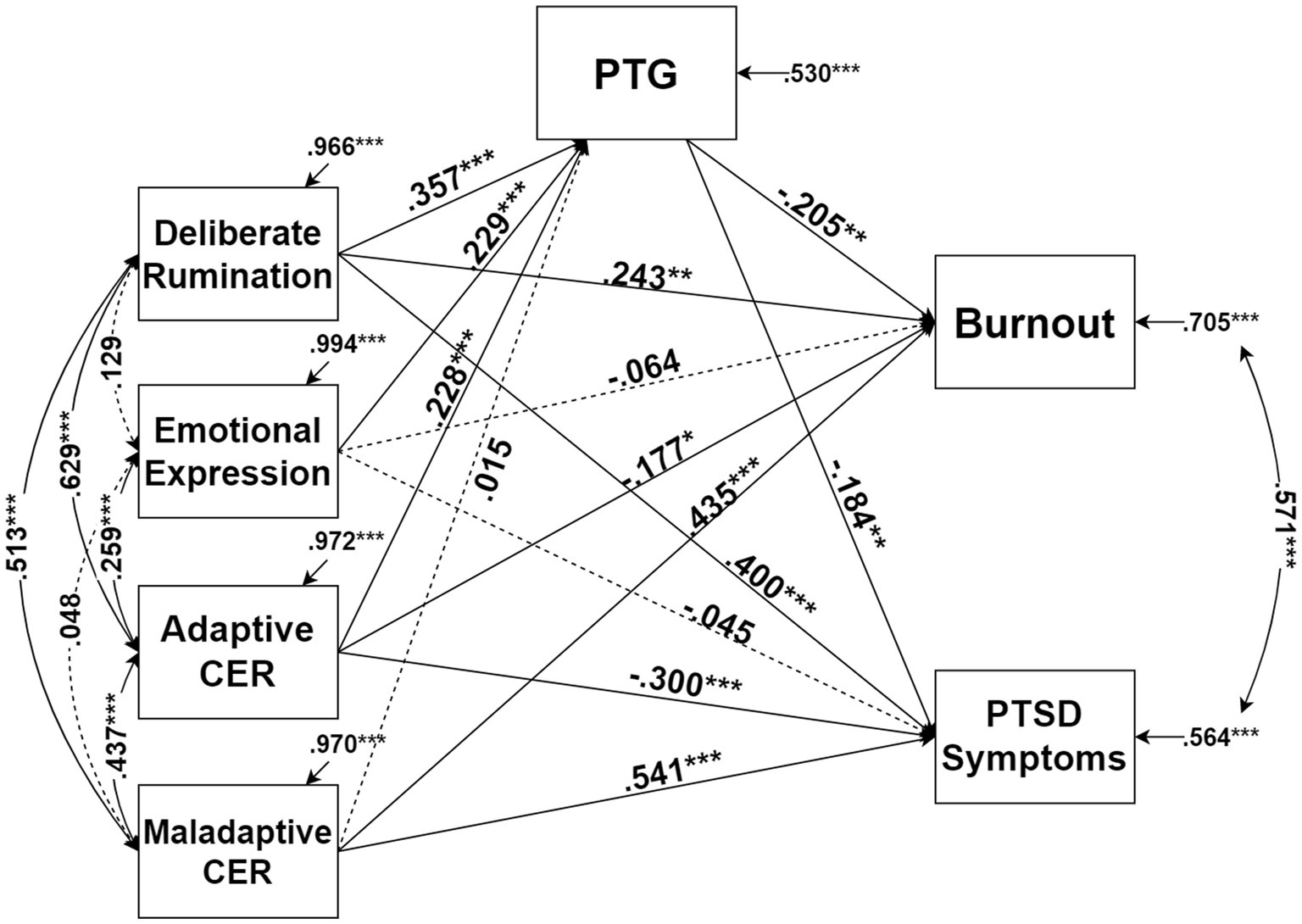
Figure 1. Result of path modeling. *p < 0.05, **p < 0.01, ***p < 0.001. All coefficients in the figure are standardized, and dotted lines are statistically insignificant coefficients.
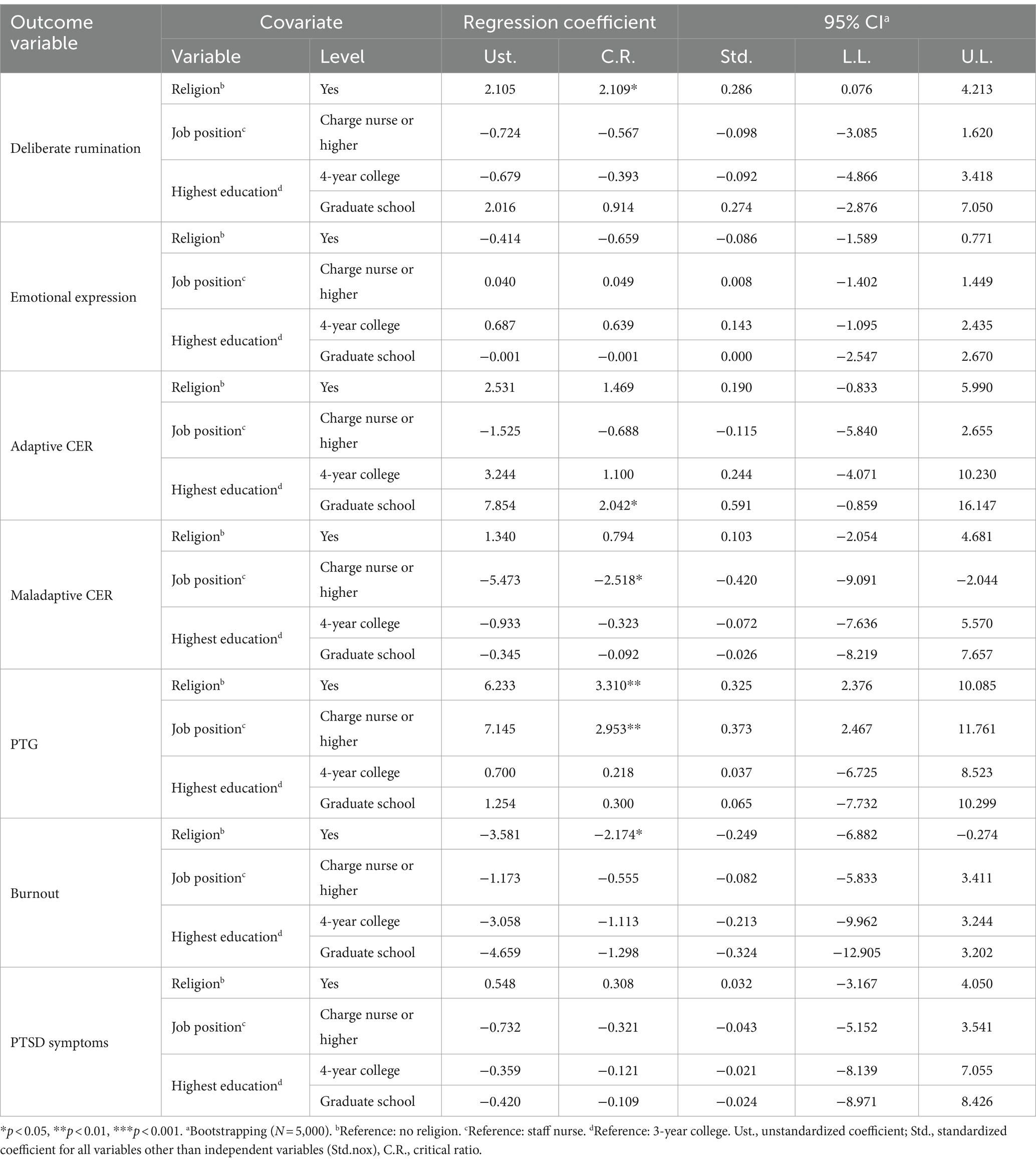
Table 5. Effects of covariates within the path model.
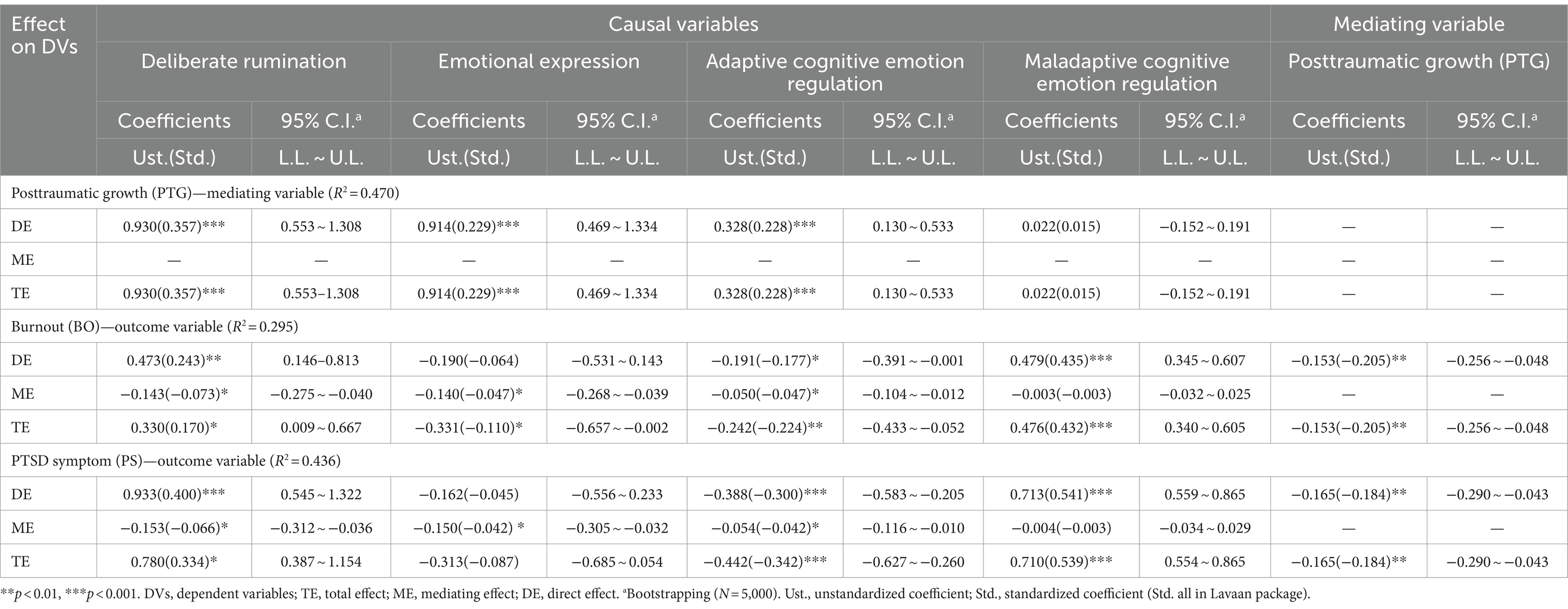
Table 6. Effect decomposition (total effect, mediating effect, and direct effect) for the path model and bootstrapping results.
4 Discussion
This study explored the variables that may influence PTG and BO in nurses during the COVID-19 pandemic and examined whether variables such as deliberate rumination, emotional expression, and adaptive CER can reduce BO and PS through the mediation of PTG. The major findings are summarized and discussed below.
First, we identified the predictors of BO, PS, and PTG. Initially, deliberate rumination, emotional expression, and adaptive CER were significant predictors of PTG. The roles of deliberate rumination (13, 23–25), emotional expression (27, 29, 30), and adaptive CER (22) as predictors of PTG have already been supported by previous studies. The findings of our study emphasize that these predictors are also essential factors in facilitating PTG in nurses. Next, deliberate rumination, adaptive CER, maladaptive CER, and PTG had significant direct effects on BO and PS. Of them, adaptive CER directly reduced BO and PS. Our result that adaptive CER alleviates job-related BO and relevant stress symptoms is consistent with previous findings (37). In other words, these are in line with the interpretation of Ehlers and Steil (41) that adaptive CER and deliberate thoughts about a trauma (or extreme stress) can modify pathological thinking patterns and thus reduce psychological distress. However, maladaptive CER increased BO and PS. Maladaptive CER related to maladaptive coping, such as avoidance and denial, prevents individuals from confronting negative experiences, thus hindering problem resolution in challenging situations. As a result, they may contribute to maintaining or even increasing psychological distress. Contrary to the hypothesis of this study, however, social support was not a significant causal variable. While many studies support the significant effect of social support, the role of social support is not simple. Recently, Saegert and Carpiano (68) revealed that social support does not solely bring positive effects but rather complex outcomes in conjunction with other factors, and some supportive relationships may have negative effects. For example, conflicts may arise when supporters become exhausted from providing sustained support over time (69). Social support arises within relationships with others, and the dynamics occurring within those relationships shape social support (70). In this regard, the social support reported by the participants may not have aligned well with the specific contextual characteristics of the pandemic. Additionally, one of the factors of social support measured in this study is the support of family, but it has been pointed out that family members may not be a helpful resource for all stressors due to the significant obligations and potential for conflict among them (70).
As opposed to our hypothesis, deliberate rumination had a direct effect on BO and PS. It is important to note that these findings are based on data collected in the unique context of the COVID-19 pandemic. During the ongoing pandemic, the healthcare system faced numerous challenges, and nurses had to deal with many difficult and stressful experiences. Therefore, it is possible that during the pandemic, engaging in more reflection and rumination about their own challenging experiences may actually have consumed their psychological energy, ultimately leading to increased BO and PS. For example, deliberately focusing on distressing memories and thoughts instead of avoiding them induces pain and stress. While deliberate rumination may lead to experiencing PTG in the long term, in the short term, deliberate rumination may not have been as effective in addressing nurses’ burnout and PTSD symptoms related to the pandemic as expected. Previous studies have already discovered that factors that had been protective prior to the COVID-19 pandemic (e.g., coping flexibility) had adverse effects during the pandemic (71). In other words, it is essential to consider the context of an individual’s situation to understand the roles of a particular variable (72). It is important to note that although deliberate rumination directly increases BO and PS, it also lowers BO and PS if PTG is increased. Given that deliberate rumination is associated with increasing PTG, it seems important to utilize deliberate rumination for patients experiencing PTSD or burnout. However, since deliberate rumination can induce pain, it appears necessary to employ it with psychological resources and abilities to endure that pain. For example, in psychotherapy, patients may find confronting psychological problems distressing, yet confronting them can be highly beneficial in resolving the problem [(e.g., 73)].
Second, the effects of adaptive CER and deliberate rumination on BO and PS were partially mediated by PTG. Deliberate rumination involves reflecting on their painful experiences and contemplating the meaning behind those experiences. This reflection may encourage people to find positive opportunities for growth amid the psychological distress caused by negative events, ultimately leading to a reduction in BO and PS. Adaptive coping is crucial in alleviating the distress associated with negative experiences and achieving PTG. In contrast to maladaptive CER, such as avoidance, catastrophizing, and self-blame, which hinder cognitive processing of negative experiences and increase BO and PS, adaptive CER encourages individuals to reinterpret events positively, accept them, and make efforts to solve problems. These effects promote experiencing PTG in the aftermath of negative events and naturally reduce BO and PS (41).
In contrast to other causal variables, the effects of emotional expression on BO and PS were completely mediated by PTG. Emotional expression relieves accumulated emotional burdens and facilitates deliberate rumination through actions such as purification (26). As a result, it is anticipated to increase PTG and reduce BO and PS. However, emotional expression alone may not be adequate in reducing negative outcomes (BO and PS). Emotional expression is a kind of self-disclosure, and self-disclosure is one of the precursors to PTG (74). If elements such as cognitive changes follow emotional expression, they can lead to positive subsequent changes (75). In other words, it can reduce BO and PS if it leads to PTG through cognitive processes such as reflection, but if PTG is not achieved, emotional expression itself (e.g., expressing pain and distress) appears to be inadequate in directly reducing BO and PS.
The finding that deliberate rumination, emotional expression, and adaptive CER facilitate PTG, which in turn leads to reduced BO and PS, carries significant clinical implications. While various psychological treatment programs have been developed and utilized to address trauma and severe stress, most of them have primarily focused on reducing maladaptive symptoms. However, there is a growing trend toward programs that not only aim to reduce maladaptive symptoms but also emphasize personal growth and maturity in response to adversity [(e.g., 76, 77)]. Nevertheless, the development and utilization of psychological therapy programs to address the challenges experienced by healthcare workers during the COVID-19 pandemic are not yet widespread. While programs for the general population are being developed and implemented extensively, there is a shortage of programs addressing the unique experiences of healthcare professionals. The results of this study, in conjunction with previous research, can serve as a basis for the development and utilization of programs aimed at managing the BO and psychological distress of frontline healthcare workers, including nurses, and facilitating their growth. By leveraging factors such as deliberate rumination, emotional expression, and adaptive CER, it is possible to prevent maladaptive symptoms and promote positive psychological growth and change. For instance, nurses can be encouraged to transform their habitual maladaptive rumination on the job into adaptive and reflective forms (78) and subsequently engage in problem-solving coping strategies. Some studies also propose methods for alleviating maladaptive rumination by facilitating the mental construction of novel scenarios in the immediate and distant future (79). Furthermore, providing nurses with opportunities to appropriately express suppressed emotions such as anger, frustration, and worry during their duties [(e.g., 80)] could increase their objective self-understanding and objective perspective on issues, thereby alleviating BO and the associated psychological distress (81).
Religion emerged as the second most influential demographic characteristic in our study. Participants who identified with a religion reported higher levels of DR and PTG and lower levels of BO compared to their non-religious counterparts. The role of religion in enhancing DR and PTG is well-supported by previous studies. For instance, religion may facilitate the PTG process by enabling individuals to find meaning in life, identify effective coping strategies and resources, and develop a revised personal narrative (82, 83). Additionally, positive religious coping, such as seeking spiritual support or maintaining a connection with God, predicted PTG following a disaster (84). Some religious doctrines view suffering not merely as a negative outcome but as an essential element for achieving purification, holiness, and preparation for the afterlife (85). Furthermore, various religions promote vocational callings or ethics (e.g., Luther’s doctrine of vocation). From this perspective, it is possible that religion facilitated individuals who suffered from a trauma or extremely stressful event to endure their suffering and deliberately ruminate the experience, thereby mitigating the impact of BO.
This study has a few limitations. First, the sample size was relatively small, given the complexity of the model being evaluated. Although most of the statistical analysis results yielded the expected or significant findings, there were instances in the model verification where some regression coefficients were statistically insignificant despite being reasonably large. Second, additional analysis was difficult for some demographic variables because of sample imbalances (e.g., female participants significantly outnumbered male participants at 233 to 14). Moreover, the marked differences in the number of participants across education levels (3-year college, 4-year college, and graduate school ranging from 22 to 194 participants) violated the strict assumption that group sizes should be equal in ANOVA. Next, the internal consistency of the Emotional Expressivity Scale was somewhat low. This could limit the interpretation of the findings of this study. It is anticipated that this may be due to the scale being developed too long ago and, therefore, not adequately measuring the construct of interest. In addition, it is necessary to include exposure to COVID-19-related trauma or infection patients as control variables, although several covariates selected through preliminary analysis were included in the model. By comparing the participants in this study with other nurses who were not exposed to trauma related to the COVID-19 pandemic or to the duties of treating infected patients, we can more accurately determine whether COVID-19 has impacted BO, PTSD, and PTG. Further research on this issue is needed. Finally, there are limitations related to the generalizability of the study findings. The cross-sectional design of this study limits the capacity to draw causal conclusions. Implementing a longitudinal design would help establish causal relationships between variables, which is essential for understanding the development of burnout, PTSD, and PTG over time. Additionally, our research is geographically confined to nurses working in South Korea. This limitation curtails the generalizability of our findings to other cultural or national contexts. A more inclusive study design involving participants from multiple countries, such as the approach taken by Chirico and Nucera (86), would potentially offer a broader perspective and enhance the applicability of the results across different settings.
Despite these limitations, however, this study has the following implications. First, it highlights that while COVID-19 can be perceived negatively, it can also serve as a catalyst for positive change. By identifying the factors that promote PTG, this study offers direction on how to intervene with healthcare professionals during the COVID-19 pandemic. Second, it emphasizes the need for psychological interventions for healthcare professionals who are dealing with the challenges of the COVID-19 pandemic. Third, a comprehensive investigation was conducted on various factors that influence not only PTG but also BO and PTSD. This study covers a broad range of factors influencing PTG, BO, and PTSD. Finally, showing that PTG can serve as a buffer against BO and PTSD, this study provides evidence that a positive psychology perspective can be useful in psychological interventions for BO and PTSD. We hope that the results of this study will be valuable in providing psychological support to healthcare workers struggling with the demands of the pandemic and, ultimately, those who have experienced trauma or extreme stress events.
5 Conclusion
This study explored the variables that may influence posttraumatic stress disorder and burnout in healthcare professionals, such as nurses, during the COVID-19 pandemic. It highlights that it has examined the pathways through which these variables lead to reduced burnout through the mediation of posttraumatic growth. By fostering the factors that promote PTG, which serves as a buffer for BO and PS in healthcare professionals, they can achieve the benefits of psychological growth and improved mental health simultaneously. It is expected that the results of this study will be valuable in providing psychological support to healthcare workers struggling with the demands of the pandemic and, ultimately, those who have undergone traumatic or highly stressful events.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Hallym Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
J-CS: Writing – original draft, Software, Project administration, Methodology, Investigation, Formal analysis, Data curation. S-KC: Writing – review & editing, Supervision, Data curation. S-YI: Writing – review & editing, Writing – original draft, Supervision, Project administration, Funding acquisition, Data curation, Conceptualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea, 2022 (NRF-2022S1A5A8055783) and Hallym University Research Fund, 2023 (HRF-202309-006).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Ganai, UJ, Sachdev, S, Bhat, N, and Bhushan, B. Associations between posttraumatic stress symptoms and posttraumatic growth elements: a network analysis. Psychol Trauma. (2022) 16:731–740. doi: 10.1037/tra0001411
Crossref Full Text | Google Scholar
3. Kangaslampi, S, Peltonen, K, and Hall, J. Posttraumatic growth and posttraumatic stress – a network analysis among Syrian and Iraqi refugees. Eur J Psychotraumatol. (2022) 13:2117902. doi: 10.1080/20008066.2022.2117902
Crossref Full Text | Google Scholar
4. Yuan, G, Park, CL, Birkeland, SR, Yip, PSY, and Hall, BJ. A network analysis of the associations between posttraumatic stress symptoms and posttraumatic growth among disaster-exposed Chinese Young adults. J Trauma Stress. (2021) 34:786–98. doi: 10.1002/jts.22673
Crossref Full Text | Google Scholar
5. Tedeschi, RG, and Calhoun, LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. (1996) 9:455–71. doi: 10.1007/BF02103658
Crossref Full Text | Google Scholar
6. Taku, K
. Relationships among perceived psychological growth, resilience and burnout in physicians. Pers. Individ. Dif. (2014) 59:120–3. doi: 10.1016/j.paid.2013.11.003
Crossref Full Text | Google Scholar
7. Lee, EJ, Cho, OY, Wang, KH, and Jang, MJ. Correlation between nurses’ posttraumatic stress disorder, depression and social stigma in nursing COVID-19 patients. J East-West Nurs Res. (2021) 27:14–21. doi: 10.14370/jewnr.2021.27.1.14
Crossref Full Text | Google Scholar
8. Yunitri, N, Chu, H, Kang, XL, Jen, H-J, Pien, L-C, Tsai, H-T, et al. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: a meta-analysis. Int J Nurs Stud. (2022) 126:104136. doi: 10.1016/j.ijnurstu.2021.104136
Crossref Full Text | Google Scholar
9. Martin, B, Kaminski-Ozturk, N, O’Hara, C, and Smiley, R. Examining the impact of the COVID-19 pandemic on burnout and stress among US nurses. J Nurs Regul. (2023) 14:4–12. doi: 10.1016/S2155-8256(23)00063-7
Crossref Full Text | Google Scholar
10. Park, HR, and Lee, SJ. Analysis of anxiety, stress and coping type of health-care worker in the COVID-19 pandemic. JKAIS. (2022) 23:57–66. doi: 10.5762/KAIS.2022.23.2.57
Crossref Full Text | Google Scholar
11. Leo, CG, Sabina, S, Tumolo, MR, Bodini, A, Ponzini, G, Sabato, E, et al. Burnout among healthcare workers in the COVID 19 era: a review of the existing literature. Front Public Health. (2021) 9:750529. doi: 10.3389/fpubh.2021.750529
Crossref Full Text | Google Scholar
12. Izdebski, Z, Kozakiewicz, A, Białorudzki, M, Dec-Pietrowska, J, and Mazur, J. Occupational burnout in healthcare workers, stress and other symptoms of work overload during the COVID-19 pandemic in Poland. Int J Environ Res Public Health. (2023) 20:2428. doi: 10.3390/ijerph20032428
Crossref Full Text | Google Scholar
13. Cui, PP, Wang, PP, Wang, K, Ping, P, Wang, P, and Chen, C. Post-traumatic growth and influencing factors among frontline nurses fighting against COVID-19. Occup Environ Med. (2021) 78:129–35. doi: 10.1136/oemed-2020-106540
Crossref Full Text | Google Scholar
14. Powell, S, Rosner, R, Butollo, W, Tedeschi, RG, and Calhoun, LG. Posttraumatic growth after war: a study with former refugees and displaced people in Sarajevo. J Clin Psychol. (2003) 59:71–83. doi: 10.1002/jclp.10117
Crossref Full Text | Google Scholar
15. Park, SR, and Im, SY. Is posttraumatic growth helpful in overcoming mental health disorders due to COVID-19?: the moderating effect of posttraumatic growth in the relationship between COVID-19 and psychological health. Front Psychol. (2021) 12:773326. doi: 10.3389/fpsyg.2021.773326
Crossref Full Text | Google Scholar
16. Hamama-Raz, Y, Hamama, L, Pat-Horenczyk, R, Stokar, YN, Zilberstein, T, and Bron-Harlev, E. Posttraumatic growth and burnout in pediatric nurses: the mediating role of secondary traumatization and the moderating role of meaning in work. Stress Health. (2021) 37:442–53. doi: 10.1002/smi.3007
Crossref Full Text | Google Scholar
17. Maercker, A, and Zoellner, T. The Janus face of self-perceived growth: toward two-component model of posttraumatic growth. Psychol Inq. (2004) 15:41–8.
Google Scholar
18. Garnefski, N, Kraaij, V, and Spinhoven, P. Negative life events, cognitive emotion regulation and emotional problems. Pers Individ Dif. (2001) 30:1311–27. doi: 10.1016/S0191-8869(00)00113-6
Crossref Full Text | Google Scholar
19. Aldao, A, Nolen-Hoeksema, S, and Schweizer, S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. (2010) 30:217–37. doi: 10.1016/j.cpr.2009.11.004
Crossref Full Text | Google Scholar
20. Ahn, HN, Lee, NB, and Joo, HS. Validation of the cognitive emotion regulation questionnaire in a Korean population. Korea J Counsel. (2013) 14:1773–94. doi: 10.15703/kjc.14.3.201306.1773
Crossref Full Text | Google Scholar
21. Im, SY, and Kwon, SM. The influence of cognitive strategies and belief systems on posttraumatic growth following relational loss. Korean J Clin Psychol. (2013) 32:567–88. doi: 10.15842/kjcp.2013.32.3.006
Crossref Full Text | Google Scholar
22. Lee, SJ, and Yang, NM. The relationship between forgiveness and posttraumatic growth of those in their 20’s who have experienced interpersonal trauma: the mediating effects of adaptive cognitive emotion regulation strategies. Stud Korean Youth. (2022) 33:31–53. doi: 10.14816/sky.2022.33.3.31
Crossref Full Text | Google Scholar
23. Romeo, A, Castelli, L, Zara, G, and Di Tella, M. Posttraumatic growth and posttraumatic depreciation: associations with core beliefs and rumination. Int J Environ Res Public Health. (2022) 19:15938. doi: 10.3390/ijerph192315938
Crossref Full Text | Google Scholar
24. Han, KA
. Prediction model for post-traumatic growth (PTG) among emergency room nurses. Doctoral dissertation. South Korea: Seoul University (2016).
Google Scholar
25. Yeo, HJ, and Park, HS. The structural analysis of variables related to posttraumatic growth among psychiatric nurses. J Korean Acad Nurs. (2020) 50:26–38. doi: 10.4040/jkan.2020.50.1.26
Crossref Full Text | Google Scholar
26. Tedeschi, RG, and Calhoun, LG. Posttraumatic growth: conceptual foundation and empirical evidence. Psychol Inq. (2004) 15:1–18. doi: 10.1207/s15327965pli1501_01
Crossref Full Text | Google Scholar
27. Morris, BA, and Shakespeare-Finch, J. Rumination, post-traumatic growth, and distress: structural equation modelling with cancer survivors. Psychooncology. (2011) 20:1176–83. doi: 10.1002/pon.1827
Crossref Full Text | Google Scholar
28. Taku, K, Calhoun, LG, Cann, A, and Tedeschi, RG. The role of rumination in the coexistence of distress and posttraumatic growth among bereaved Japanese university students. Death Stud. (2008) 32:428–44. doi: 10.1080/07481180801974745
Crossref Full Text | Google Scholar
29. Manne, S, Ostroff, J, Winkel, G, Goldstein, L, Fox, K, and Grana, G. Posttraumatic growth after breast cancer: patient, partner, and couple perspectives. Psychosom Med. (2004) 66:442–54. doi: 10.1097/01.psy.0000127689.38525.7d
Crossref Full Text | Google Scholar
30. Song, H, and Lee, YS. The relation between emotional clarity and posttraumatic growth: emotional expression and emotional regulation style as mediating variable. Korean J Counseli Psychother. (2012) 24:891–910.
Google Scholar
31. Schaefer, JA, and Moos, RH. Life crises and personal growth In: B Carpenter
, editor. Personal coping: theory, research, and application. Westport, CT: Praeger (1992). 149–70.
Google Scholar
32. Ogińska-Bulik, N, Gurowiec, PJ, Michalska, P, and Kędra, E. Prevalence and determinants of secondary posttraumatic growth following trauma work among medical personnel: a cross sectional study. Eur J Psychotraumatol. (2021) 12:1876382. doi: 10.1080/20008198.2021.1876382
Crossref Full Text | Google Scholar
33. Aliche, JC, Ifeagwazi, CM, Onyishi, IE, and Mefoh, PC. Presence of meaning in life mediates the relations between social support, posttraumatic growth, and resilience in young adult survivors of a terror attack. J Loss Trauma. (2019) 24:736–49. doi: 10.1080/15325024.2019.1624416
Crossref Full Text | Google Scholar
34. Ning, J, Tang, X, Shi, H, Yao, D, Zhao, Z, and Li, J. Social support and posttraumatic growth: a meta-analysis. J Affect Disord. (2023) 320:117–32. doi: 10.1016/j.jad.2022.09.114
Crossref Full Text | Google Scholar
35. Žukauskienė, R, Kaniušonytė, G, Bergman, LR, Bakaitytė, A, and Truskauskaitė-Kunevičienė, I. The role of social support in identity processes and posttraumatic growth: a study of victims of intimate partner violence. J Interpers Violence. (2021) 36:7599–624. doi: 10.1177/0886260519836785
Crossref Full Text | Google Scholar
36. Maslach, C, and Jackson, SE. The measurement of experienced burnout. J Organ Behav. (1981) 2:99–113. doi: 10.1002/job.4030020205
Crossref Full Text | Google Scholar
37. Baik, DI, and Kim, OS. The effects of cognitive emotion regulation strategies on the professional quality of life in hospital nurses. JKAIS. (2020) 21:212–21. doi: 10.5762/KAIS.2020.21.10.212
Crossref Full Text | Google Scholar
38. Muñoz-Navarro, R, Malonda, E, Llorca-Mestre, A, Cano-Vindel, A, and Fernández-Berrocal, P. Worry about COVID-19 contagion and general anxiety: moderation and mediation effects of cognitive emotion regulation. J Psychiatr Res. (2021) 137:311–8. doi: 10.1016/j.jpsychires.2021.03.004
Crossref Full Text | Google Scholar
39. Cann, A, Calhoun, LG, Tedeschi, RG, and Solomon, DT. Posttraumatic growth and depreciation as independent experiences and predictors of well-being. J Loss Trauma. (2010) 15:151–66. doi: 10.1080/15325020903375826
Crossref Full Text | Google Scholar
40. Feingold, JH, Hurtado, A, Feder, A, Peccoralo, L, Southwick, SM, Ripp, J, et al. Posttraumatic growth among health care workers on the frontlines of the COVID-19 pandemic. J Affect Disord. (2022) 296:35–40. doi: 10.1016/j.jad.2021.09.032
Crossref Full Text | Google Scholar
41. Ehlers, A, and Steil, R. Maintenance of intrusive memories in posttraumatic stress disorder: a cognitive approach. Behav Cogn Psychother. (1995) 23:217–49. doi: 10.1017/S135246580001585X
Crossref Full Text | Google Scholar
42. Paunovic, N, and Öst, L-G. Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behav Res Ther. (2001) 39:1183–97. doi: 10.1016/s0005-7967(00)00093-0
Crossref Full Text | Google Scholar
43. Smyth, JM, Hockemeyer, JR, and Tulloch, H. Expressive writing and post-traumatic stress disorder: effects on trauma symptoms, mood states, and cortisol reactivity. Br J Health Psychol. (2008) 13:85–93. doi: 10.1348/135910707X250866
Crossref Full Text | Google Scholar
44. Campbell-Sills, L, Barlow, DH, Brown, TA, and Hofmann, SG. Effects of suppression and acceptance on emotional responses of individuals with anxiety and mood disorders. Behav Res Ther. (2006) 44:1251–63. doi: 10.1016/j.brat.2005.10.001
Crossref Full Text | Google Scholar
45. Kashdan, TB, and Breen, WE. Social anxiety and positive emotions: a prospective examination of a self-regulatory model with tendencies to suppress or express emotions as a moderating variable. Behav Ther. (2008) 39:1–12. doi: 10.1016/j.beth.2007.02.003
Crossref Full Text | Google Scholar
46. Park, HJ
. Emotional labour, emotional expression and burnout of clinical nurses. J Korean Acad Nurs Adm. (2009) 15:225–32.
Google Scholar
47. Im, SY
. Psychometric properties of posttraumatic growth scale-extended version (PTGI-X): reexamination of the factor structure and usefulness of the Korean translated scale. Clin Psychol Korea. (2023) 9:161–81. doi: 10.15842/CPKJOURNAL.PUB.9.1.161
Crossref Full Text | Google Scholar
48. Kline, RB
. Principles and practice of structural equation modeling. 4th ed. New York, NY: Guildford (2015).
Google Scholar
49. Tedeschi, RG, Cann, A, Taku, K, Senol-Durak, E, and Calhoun, LG. The posttraumatic growth inventory: a revision integrating existential and spiritual change. J Trauma Stress. (2017) 30:11–8. doi: 10.1002/jts.22155
Crossref Full Text | Google Scholar
50. Schaufeli, WB, Desart, S, and De Witte, H. Burnout assessment tool (BAT) – development, validity, and reliability. Int J Environ Res Public Health. (2019) 17:9495. doi: 10.3390/ijerph17249495
Crossref Full Text | Google Scholar
51. Cho, SH
. A preliminary validation study for the Korean version of the burnout assessment tool (K-BAT). Korean J Ind Organ Psychol. (2020) 33:461–99. doi: 10.24230/kjiop.v33i4.461-499
Crossref Full Text | Google Scholar
52. Blevins, CA, Weathers, FW, Davis, MT, Witte, TK, and Domino, JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. (2015) 28:489–98. doi: 10.1002/jts.22059
Crossref Full Text | Google Scholar
53. Lee, DH, Ku, MJ, Kwon, WH, and Kim, SH. A study on reliability and validity of the Korean version of PCL-5 (posttraumatic stress disorder checklist for DSM-5) for adults. Korean J Counsel Psychother. (2020) 32:559–82. doi: 10.23844/kjcp.2020.05.32.2.559
Crossref Full Text | Google Scholar
54. Lee, DH, Lee, DH, Kim, SH, and Jung, DS. A longitudinal validation study of the Korean version of PCL-5(post-traumatic stress disorder checklist for DSM-5). Mast Your Disab. (2022) 28:187–217. doi: 10.20406/kjcs.2022.5.28.2.187
Crossref Full Text | Google Scholar
55. Morrison, K, Su, S, Keck, M, and Beidel, DC. Psychometric properties of the PCL-5 in a sample of first responders. J Anxiety Disord. (2021) 77:102339. doi: 10.1016/j.janxdis.2020.102339
Crossref Full Text | Google Scholar
56. Wortmann, JH, Jordan, AH, Weathers, FW, Resick, PA, Dondanville, KA, Hall-Clark, B, et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. (2016) 28:1392–403. doi: 10.1037/pas0000260
Crossref Full Text | Google Scholar
57. Ahmadi, A, Galusha, JM, Ponder, WN, Carbajal, J, Schuman, DL, Whitworth, J, et al. Validation of the PCL-5, PHQ-9, and GAD-7 in a sample of first responders. J Occup Environ Med. (2023) 65:467–76. doi: 10.1097/JOM.0000000000002823
Crossref Full Text | Google Scholar
58. Ahmadi, A, Ponder, WN, Carbajal, J, Schuman, DL, Whitworth, J, Yockey, RA, et al. Validation of the PCL-5, PHQ-9, and GAD-7 in a sample of veterans. J Occup Environ Med. (2023) 65:643–54. doi: 10.1097/JOM.0000000000002898
Crossref Full Text | Google Scholar
59. Cann, A, Calhoun, LG, Tedeschi, RG, Triplett, KN, Vishnevsky, T, Lindstrom, C, et al. Assessing posttraumatic cognitive processes: the event related rumination inventory. Anxiety Stress Coping. (2011) 24:137–56. doi: 10.1080/10615806.2010.529901
Crossref Full Text | Google Scholar
60. Ahn, HN, Joo, HS, Min, JW, and Sim, KS. Validation of the event related rumination inventory in a Korean population. CBTK. (2013) 13:149–72.
Google Scholar
61. Kring, AM, Smith, DA, and Neale, JM. Individual differences in dispositional expressiveness: development and validation of the emotional expressivity scale. J Pers Soc Psychol. (1994) 66:934–49. doi: 10.1037/0022-3514.66.5.934
Crossref Full Text | Google Scholar
62. Han, JW
. The influences of emotional expressivity on physical health and subjective well-being. Master’s dissertation, South Korea Seoul University (1997).
Google Scholar
63. Zimet, GD, Dahlem, NW, Zimet, SG, and Farley, GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
Crossref Full Text | Google Scholar
64. Yune, HS, and Oh, KJ. The effect of social support on parenting stress among families in poverty: focused on children’s age and environmental risk factors. Korean J Wom Psychol. (2010) 15:673–89. doi: 10.18205/kpa.2010.15.4.007
Crossref Full Text | Google Scholar
66. Hair, J, Black, WC, Babin, BJ, and Anderson, RE. Multivariate data analysis. 7th ed. Upper saddle River, NJ: Pearson Education International (2010).
Google Scholar
67. Curran, PJ, West, SG, and Finch, JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods. (1996) 1:16–29. doi: 10.1037/1082-989X.1.1.16
Crossref Full Text | Google Scholar
68. Saegert, S, and Carpiano, RM. Social support and social capital: a theoretical synthesis using community psychology and community sociology approaches In: MA Bond, I Serrano-García, CB Keys, and M Shinn, editors. APA handbook of community psychology. vol. 1: theoretical foundations, core concepts, and emerging challenges. Washington, DC: American Psychological Association (2017). 295–314.
Google Scholar
69. Kohn-wood, LP, and Wilson, MN. The context of caretaking in rural areas: family factors influencing the level of functioning of serious mentally ill patients living at home. Am J Community Psychol. (2005) 36:1–13. doi: 10.1007/s10464-005-6229-2
Crossref Full Text | Google Scholar
70. Kloos, B, Hill, J, Thomas, E, Case, AD, Scott, VC, and Wandersman, A. Community psychology: linking individuals and communities. Washington, DC: American Psychological Association (2020).
Google Scholar
71. Sim, JC, and Im, SY. The impact of COVID-19 on mental health and posttraumatic growth of Korean college students: a mixed method study examining the moderating role of coping flexibility and sense of community. Front Psychol. (2023) 14:1200570. doi: 10.3389/fpsyg.2023.1200570
Crossref Full Text | Google Scholar
72. Galinha, IC, and Pais-Ribeiro, JL. Cognitive, affective and contextual predictors of subjective wellbeing. IJW. (2011) 2:34–53. doi: 10.5502/ijw.v2i1.3
Crossref Full Text | Google Scholar
73. Moeseneder, L, Ribeiro, E, Muran, JC, and Caspar, F. Impact of confrontations by therapists on impairment and utilization of the therapeutic alliance. Psychother Res. (2019) 29:293–305. doi: 10.1080/10503307.2018.1502897
Crossref Full Text | Google Scholar
74. Tedeschi, RG, Shakespeare-Finch, J, Taku, K, and Calhoun, LG. Posttraumatic growth: theory, research, and applications. New York, NY: Routledge (2018).
Google Scholar
75. Garfield, SL
. Psychotherapy: an eclectic-integrative approach. New York, NY: John Wiley & Sons (1995).
Google Scholar
76. Bae, KR, So, WY, and Jang, S. Effects of a post-traumatic growth program on young Korean breast cancer survivors. Healthcare. (2023) 11:140. doi: 10.3390/healthcare11010140
Crossref Full Text | Google Scholar
77. Im, SY
. Efficacy of the group therapy to facilitate posttraumatic growth on relational loss-sufferers. CBTK. (2014) 14:339–58.
Google Scholar
78. Watkins, ER, and Nolen-Hoeksema, S. A habit-goal framework of depressive rumination. J Abnorm Psychol. (2014) 123:24–34. doi: 10.1037/a0035540
Crossref Full Text | Google Scholar
79. Zhou, HX, Chen, X, Shen, YQ, Li, L, Chen, NX, Zhu, ZC, et al. Rumination and the default mode network: Meta-analysis of brain imaging studies and implications for depression. Neuroimage. (2020) 206:116287. doi: 10.1016/j.neuroimage.2019.116287
Crossref Full Text | Google Scholar
80. Zhan, J, Yu, S, Cai, R, Xu, H, Yang, Y, Ren, J, et al. The effects of written catharsis on anger relief. Psych J. (2021) 10:868–77. doi: 10.1002/pchj.490
Crossref Full Text | Google Scholar
81. Lieberman, MD, Eisenberger, N, Crockett, MJ, Tom, SM, Pfeifer, JH, and Way, BM. Putting feeling into words: affect labeling disrupts amygdala activity in response to affective stimuli. Psychol Sci. (2007) 18:421–8. doi: 10.1111/j.1467-9280.2007.01916.x
Crossref Full Text | Google Scholar
82. Ai, AL, Hall, D, Pargament, K, and Tice, TN. Posttraumatic growth in patients who survived cardiac surgery: the predictive and mediating roles of faith-based factors. J Behav Med. (2013) 36:186–98. doi: 10.1007/s10865-012-9412-6
Crossref Full Text | Google Scholar
83. Shaw, A, Joseph, S, and Linley, PA. Religion, spirituality, and posttraumatic growth: a systematic review. Ment Health Relig Cult. (2005) 8:1–11. doi: 10.1080/1367467032000157981
Crossref Full Text | Google Scholar
84. Chan, CS, and Rhodes, JE. Religious coping, posttraumatic stress, psychological distress, and posttraumatic growth among female survivors four years after hurricane Katrina. J Trauma Stress. (2013) 26:257–65. doi: 10.1002/jts.21801
Crossref Full Text | Google Scholar
85. Calhoun, LG, and Tedeschi, RG. The foundations of posttraumatic growth: an expanded framework In: LG Calhoun and RG Tedeschi, editors. Handbook of posttraumatic growth: research and practice. Mahwah: Lawrence Erlbaum Associates (2006). 3–23.
Google Scholar
86. Chirico, F, and Nucera, G. Tribute to healthcare operators threatened by COVID-19 pandemic. J. Health. Soc. Sci. (2020) 5:165–8. doi: 10.19204/2020/trbt1
Crossref Full Text | Google Scholar
link




More Stories
Recovery-oriented and trauma-informed care for people with mental disorders to promote human rights and quality of mental health care: a scoping review | BMC Psychiatry
Best Healthcare Destinations for AI-Powered Post-Trauma Recovery | Medical Tourism Magazine | Medical Travel
New Study Examines Patient Suicide and Its Toll on Providers