Demographic characteristics
Table 1 shows the basic demographic details of the study participants.
According to Table 1, most study participants were female, 57% (n = 62), while males comprised 42% (n = 46). The age range of participants was from 21 to 65 years old, with a mean age of 33 (SD = 7.9) years old, and the majority aged below 40 years old, 80% (n = 87). Almost half of the participants were from Blantyre, 46% (n = 50). Most respondents, 77% (n = 84), were from city referral hospitals of Blantyre and Lilongwe, while only 23% (n = 25) were from the district hospitals of Mangochi and Karonga).
Prevalence of COVID-19-related depression, anxiety and PTSD
Table 2. shows the point prevalence of COVID-19-related depression segregated by demographic factors.
The results of this study (Table 2) indicated an overall high prevalence of COVID-19-related depression (31%; CI [23, 41]), anxiety (30%; CI [22, 40]) and PTSD (25%; CI [17, 34]) among health care workers. However, most respondents had mild depression (18.4%) or anxiety (20.2%), as highlighted in Fig. 1.
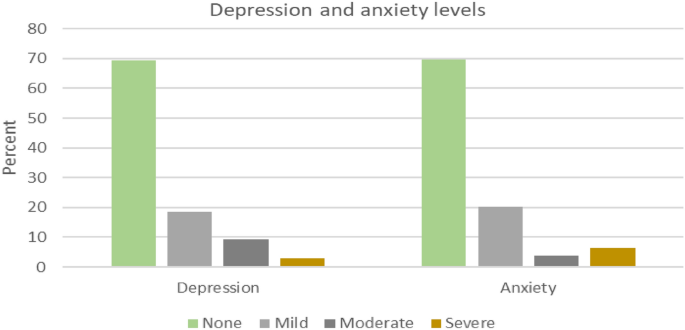
Levels of depression and anxiety for sampled health care workers.
A high proportion of depression was observed in Blantyre (n = 20, 40%) and among female health workers (n = 24, 39%). On the other hand, a high proportion of anxiety was observed in Lilongwe (n = 15, 44%) and among female health workers (n = 22, 35%). Furthermore, a high proportion of PTSD incidence was observed in Lilongwe (n = 12, 35%) and among female health workers (n = 18, 29%).
Despite the observed differences in depression, anxiety and PTSD prevalence for different variable groups, the regression results reveal that these differences are not statistically significant (Table 3).
The qualitative data analysis revealed three main themes that encapsulate the experiences and challenges faced by healthcare workers in Malawi during the COVID-19 pandemic: 1) Mental health symptoms and emotional distress, 2) Impact on work and personal life, and 3) Stigma and discrimination.
Mental health symptoms and emotional distress
The healthcare workers across the four districts reported experiencing a wide range of concerning mental health symptoms related to depression, anxiety, and posttraumatic stress disorder (PTSD). Regarding depressive symptoms, many workers described persistent sadness, hopelessness, loss of interest in everyday activities, fatigue, worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicide. The healthcare workers highlighted excessive worry, restlessness, difficulty relaxing, irritability, muscle tension, sleep disturbances, and panic attacks as some of the anxiety-related symptoms they had been experiencing. Additionally, the workers reported PTSD-associated symptoms, including unwanted distressing memories of treating COVID-19 patients and emotional and physical reactions when reminded of traumatic pandemic experiences. This avoidance of people or situations triggers recollections of trauma, hypervigilance, and exaggerated startle response. “Memories of the dead from Covid-19 haunted most of us. Most of the night, I failed to sleep. Some health workers reported the same to me. They would come for help, but I could only give them sleeping pills” (Matron, Karonga). “Sometimes, you just wish you could just shut down. Just forget everything. It was too much for us; too much sadness” (Matron, Lilongwe).
According to the healthcare workers’ accounts, these mental health symptoms had persisted for several months since the onset of the COVID-19 pandemic and significantly impacted their daily functioning and quality of life. Some workers reported being unable to get out of bed in the morning due to depression, while others described intense anxiety preventing them from being able to focus at work. The intrusive re-experiencing symptoms of PTSD were causing some workers substantial distress. Several workers tearfully recalled traumatic events such as holding the hands of dying COVID patients. These traumatic memories now haunted the healthcare workers, causing sleep disturbances and emotional anguish. In addition, traumatic experiences related to COVID-19 patient care also led to PTSD symptoms, such as intrusive memories and emotional numbing. A nurse in Lilongwe recounted, “I can still hear the sound of the ventilator alarms and see the faces of the patients who passed away. It is like a constant reminder of the tragedy we witnessed.“
In addition to the associated symptoms, healthcare workers also described profound emotional distress from their experiences of rapid patient deterioration and death in COVID-19 cases. As one clinician from Mangochi district poignantly recounted: “Most people say medical personnel are used to that, but with that disease, it is not easy to see people who were okay suddenly got the disease, it gets worse, and suddenly they die; it was too much to accept it.” (Clinician, Mangochi). Further, anxiety symptoms were also prevalent, with healthcare workers mentioning excessive worry, restlessness, and sleep disturbances. A clinician in Karonga remarked, “I would lie awake at night, my mind racing with thoughts of all the patients I could not save and the constant fear of bringing the virus home to my family.“
These clinicians’ accounts provide insight into the trauma and moral injury inflicted on healthcare workers by the stark severity and frequent fatalities of COVID-19. It exemplifies the psychological impact of experiencing rapid patient declines and deaths first-hand, sometimes without adequate resources to prevent grievous outcomes. The sentiment expressed by this frontline worker in Mangochi district was similarly echoed by many others who struggled to come to terms with the sudden loss of life amongst their patients. One nurse from Karonga shared, “I felt so overwhelmed and helpless seeing patients deteriorate despite our best efforts. It was like a never-ending nightmare.” These experiences likely contributed to the substantial burden of depressive, anxiety, and PTSD symptoms endorsed by the healthcare workers amid Malawi’s COVID-19 response.
Impact on work and personal life
Participants reported that frontline health workers were overwhelmed with work due to an increase in patient numbers and a reduction in the number of health workers. However, in Mangochi, respondents reported a general decrease in patient numbers, approximately from 60 patients per day to 30 per day; this did not translate to a lower workload since there was also a reduction in health workers for various reasons such as unexplained absenteeism, sickness and transfers. One nurse from Mangochi shared, “We were stretched thin, working endless hours with little rest. It was physically and emotionally draining.” The same applied to Karonga, where healthcare workers were expected to work continuously for two weeks, followed by a week’s holiday. This work overload may have contributed to “burnout”, as reported by most participants. “The workload has increased, as you know. The pandemic, especially the second wave, hit us hard, so the workload just increased suddenly” (Nurse, Karonga).
Respondents also reported reduced face-to-face interaction with fellow workers, mainly due to new work protocols. COVID-19 measures, such as social distancing and the frequent use of Personal Protective Equipment (PPE, reduced their sense of connectedness. In addition, work output was negatively affected; participants attributed this to increased absenteeism, attrition and application of leave days, which was attributed to workers’ fear of contracting COVID-19 at the workplace. Participants reported more panic and fear during the first wave than in the second since the healthcare workers might have developed strategies and coping mechanisms. “… so, there was less panic and fear in responding to the second wave because we had now learnt what we should do” (Matron, Lilongwe). Further, the fear of contracting the virus and infecting loved ones also took a toll on healthcare workers’ family dynamics. “I had to isolate myself from my family for months, unable to hug my children or comfort them when they needed me the most. It was a painful sacrifice” (Clinician, Blantyre).
The COVID-19 pandemic also disrupted healthcare workers’ family relationships and social connections in numerous ways. Many participants described the constant terror of spreading the virus to loved ones. This led some workers to agonise to isolate themselves entirely from family to avoid potential transmission. One matron from Lilongwe explained: “There was a time I thought I should send my wife and children home so that I should remain alone.” Sacrificing these crucial family bonds during an already stressful period exacted deep emotional pain, leaving workers feeling alone when support was most needed. Even for those who did not entirely self-isolate, the spectre of viral transmission strained family dynamics. Workers reported feeling unable to embrace loved ones, attend important events like weddings and funerals, or find comfort in casual physical affection. Families are vital for mental health; this constant stress and distance in relationships took a substantial psychological toll. Further, healthcare workers also expressed grief over the loss of colleagues and the impact on team morale. “Losing our coworkers to COVID-19 was devastating. It felt like a part of our family was gone, and the void they left behind was immense” (Nurse, Karonga).
Stigma and discrimination
Healthcare workers faced significant stigma and discrimination from their communities due to their occupation. Many reported instances of social isolation, harassment, and even violence. One nurse from Mangochi recounted, “People would yell at me on the street, calling me a virus carrier. They would cross the road to avoid passing by me as if I were a walking biohazard.” The stigma also extended to their living situations, with some healthcare workers being evicted from their homes by landlords who feared they would spread the virus. “I was kicked out of my rental apartment because the landlord found out I worked in a COVID-19 unit. I had nowhere to go and felt utterly betrayed” (Nurse, Lilongwe).
Participants described pervasive stigma from the community that damaged their social lives and sense of self. Many healthcare workers felt ostracised by the communities they sought to serve. Friends and neighbours avoided interacting with them in public due to transmission fears. This social stigma made healthcare workers increasingly isolated from previous social supports. For some healthcare workers, the stigma escalated to threats of physical violence. Multiple accounts emerged of community members throwing rocks at visiting health workers or barricading them from entering villages to administer vaccines. Workers feared that misinformation linking them to virus transmission had provoked this aggression. The social rejection, housing discrimination, and violence described by participants illustrate the heavy emotional toll of stigma during public health crises. Health workers felt hurt and afraid in the very communities they sacrificed to protect. This mistreatment exacerbated an already isolating and stressful pandemic working environment.
Many healthcare workers experienced self-stigma and were reluctant to seek mental health support despite the availability of some psychosocial support services. They feared further stigmatisation from colleagues who might perceive them as weak or incapable of handling their job responsibilities. A clinician in Blantyre admitted, “I was afraid to admit I needed mental health support. I did not want my colleagues to think I was weak or incapable of handling my job.” In addition to the fear of stigmatisation, many workers were unaware of the existence of in-house counselling or support services. Heavy workloads also left them little time to pursue such services, even when they knew their availability.
link






More Stories
Recovery-oriented and trauma-informed care for people with mental disorders to promote human rights and quality of mental health care: a scoping review | BMC Psychiatry
Best Healthcare Destinations for AI-Powered Post-Trauma Recovery | Medical Tourism Magazine | Medical Travel
New Study Examines Patient Suicide and Its Toll on Providers